Grandmother-of-seven with a broken arm died after physician associate's 'mistake' during an 'unnecessary medical procedure'
A grandmother in hospital with a broken arm died from an infection after an ‘unnecessary medical procedure’ was carried out by a physician associate.
Susan Pollitt, 77, was admitted to Royal Oldham Hospital, Greater Manchester, in July last year.
She died five days later after a procedure to remove excess fluid from her abdomen was botched by a physician associate (PA) – healthcare medics with just two years training.
The tragedy comes as criticism grows around the NHS’s reliance on PAs – healthcare workers who do not have a medical degree but are employed to support doctors.
PAs are not qualified to diagnose patients, prescribe drugs or order scans, and are meant to be constantly monitored by a doctor. Yet in an increasing number of cases, hospitals use PAs to cover for a lack of doctors in wards that range from gynaecology to A&E.

Susan Pollitt, 77, (pictured) was admitted to Royal Oldham Hospital, Greater Manchester, in July last year

The tragedy comes as criticism grows around the NHS ’s reliance on PAs – healthcare workers who do not have a medical degree but are employed to support doctors. Pictured: File photo of The Royal Oldham Hospital
A group of senior doctors are now suing the General Medical Council (GMC), the doctors’ regulator, for failing to set out clear rules over which medical tasks PAs are allowed to do.
Lawyers representing the group, who call themselves Anaesthetists United, wrote to the GMC last week accusing it of ‘acting unlawfully’ by failing to create strict regulations on the roles of PAs and anaesthesia associates (AAs) – PAs who assist with sedating patients before surgery.
The group claims that AAs are being allowed to put patients to sleep without a doctor present. They also claim that, in some hospitals, AAs are sedating children without the supervision of a doctor.
‘The issue is not that associates are working in hospitals but that what they do is so completely undefined,’ said consultant anaesthetist Dr Richard Marks, who leads the group.
‘Our court case is about setting limits on their responsibilities, as well as establishing what consent patients have to give and what level of supervision is required.’
The NHS, which already has about 3,500 PAs, plans to recruit some 10,000 by 2038 to free up time for doctors and nurses.
The Mail on Sunday has been raising the alarm for the past year as part of our Rein In The Physician Associates campaign. An investigation by this newspaper this year revealed dozens of cases where PAs had been allowed to cover doctors’ shifts and care for severely unwell patients.
In response, the Government pledged to end the practice and ensure patients are ‘cared for by the right, qualified healthcare professional’.

Mrs Pollitt’s daughter Kate said the family had been left ‘broken’, adding: ‘Things need to change.’ Pictured: Susan with her husband Roy

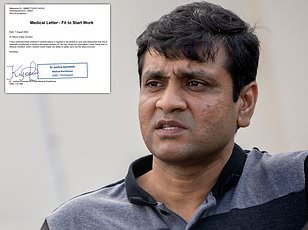
Ms Pollitt's death was the result of ‘an unnecessary medical procedure’ and was contributed to by neglect, senior coroner Joanne Kearsley concluded following an inquest at Rochdale Coroner's Court (file photo)
But experts say the death of grandmother-of-seven Mrs Pollitt is proof that strict regulations must be introduced to stop PAs carrying out tasks for which they are not qualified.
Her death was the result of ‘an unnecessary medical procedure’ and was contributed to by neglect, senior coroner Joanne Kearsley concluded last week following an inquest at Rochdale Coroners’ Court.
When Mrs Pollitt arrived in hospital, a decision was made to remove excess fluid from her abdomen – known as an ascitic drain – due to another health condition.
The procedure involves cutting the abdomen to insert a plastic tube and stitching a cuff to the skin around it.
In Mrs Pollitt’s case it was carried out by an unnamed PA – despite there being ‘no adequate procedure for ensuring PAs were competent and capable of undertaking’ this task, said Ms Kearsley.
Ascitic drains should be left in for no more than six hours – Mrs Pollitt’s was there for nearly a day. She developed an infection called bacterial peritonitis and died five days later.
‘On the balance of probabilities, she would not have died had the drain not been inserted for 21 hours,’ said Ms Kearsley.
She later added: ‘There is no national framework as to how physician associates should be trained, supervised and deemed competent. This is placing patients, physician associates and their employers at risk.’
Mrs Pollitt’s daughter Kate said the family had been left ‘broken’, adding: ‘Things need to change.’
The GMC said: ‘Anaesthetists United’s lawyers have informed us of their intention to seek a judicial review. We are considering their claims and will respond in due course.’