Abstract
Saphenous vein graft aneurysm (SVGA) is one of the chronic complications after coronary aorta bypass grafting (CABG) and may be caused by atherosclerosis-like phenomena of the vein graft, weakness around the vein valve, rupturing of the suture of the graft anastomosis, or perioperative graft injury. We describe a case of a large, growing saphenous vein graft aneurysm that was followed serially by chest radiography and computed tomography. Eighteen years after CABG, an SVGA (23 × 24 mm) was incidentally detected. The patient was asymptomatic and was followed conservatively. Four years later, coronary computed tomographic angiography showed that the giant aneurysm had grown to 52.1 by 63.8 mm and revealed a second, smaller aneurysm. Finally, the SVG was ultimately resected without bypass via off-pump surgery. Therefore, this case suggested that aggressive treatment that includes surgical intervention should be considered before the aneurysm becomes larger, even if it is asymptomatic.
1 Introduction
Saphenous vein graft aneurysm (SVGA) is one of the chronic complications after coronary artery bypass graft (CABG) surgery [1,2]. However, a serially-observed case of giant saphenous vein graft aneurysm after coronary artery bypass surgery is rare.
We describe a case of a large, growing SVGA that was followed by chest radiography (Figure 1) and computed tomography (CT) (Figure 2). The SVGA was ultimately resected without bypass via off-pump surgery.
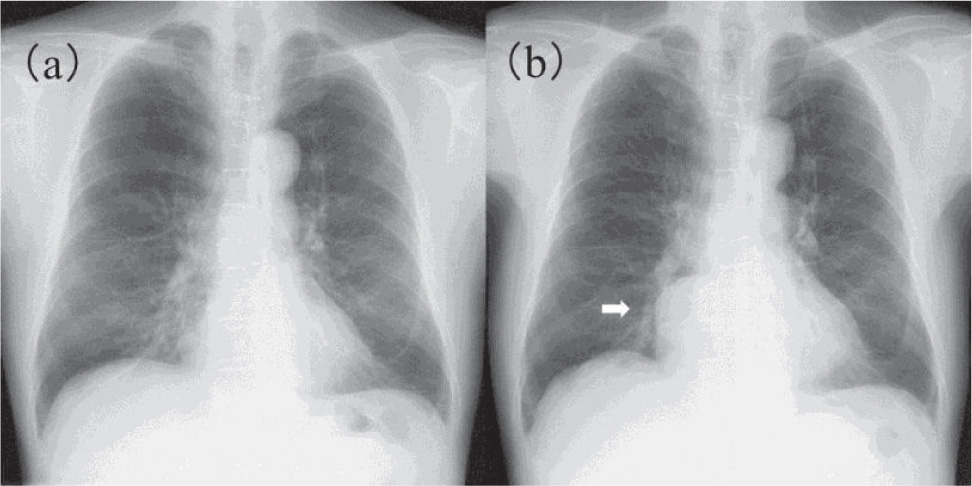
Chest radiography findings.
Chest radiography showed no abnormal shadow.
Four years later, a large mass was observed in the right inferior mediastinum (arrow).
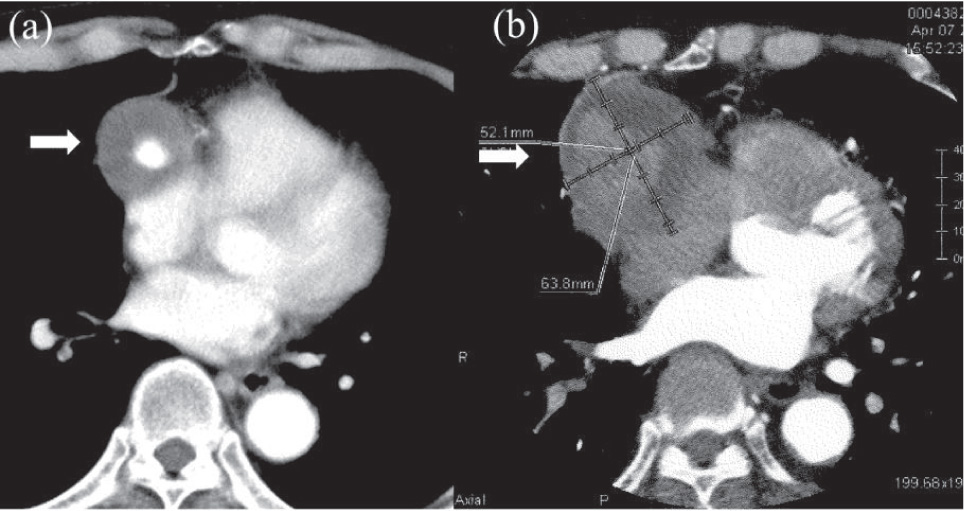
Vein graft aneurysm progression over 4 years.
Chest computed tomography showed a small vein aneurysm near the proximal anastomoses (a) and another large aneurysm around distal anastomoses (b, arrows).
2 Case report
We present a case of 70-year-old man who underwent coronary arteriography first at 48 years of age that revealed severe triple-vessel disease. Hence, CABG of the left internal thoracic artery to left anterior descending artery and of the aorta to the right coronary artery (RCA) (the 4AV branch via the SVG) were performed.
Eighteen years later, a vein graft aneurysm (23 × 24 mm) was incidentally detected where the SVG was anastomosed to the RCA (Figures 1a and 2a). The patient was asymptomatic and was followed conservatively. Several months later, he experienced acute coronary syndrome (ACS) and underwent emergency coronary arteriography. The surgery revealed that RCA and the SVG to the RCA were totally occluded with a giant graft aneurysm (Figure 3). Percutaneous coronary intervention was unsuccessful; therefore, conservative medical treatment was administered.
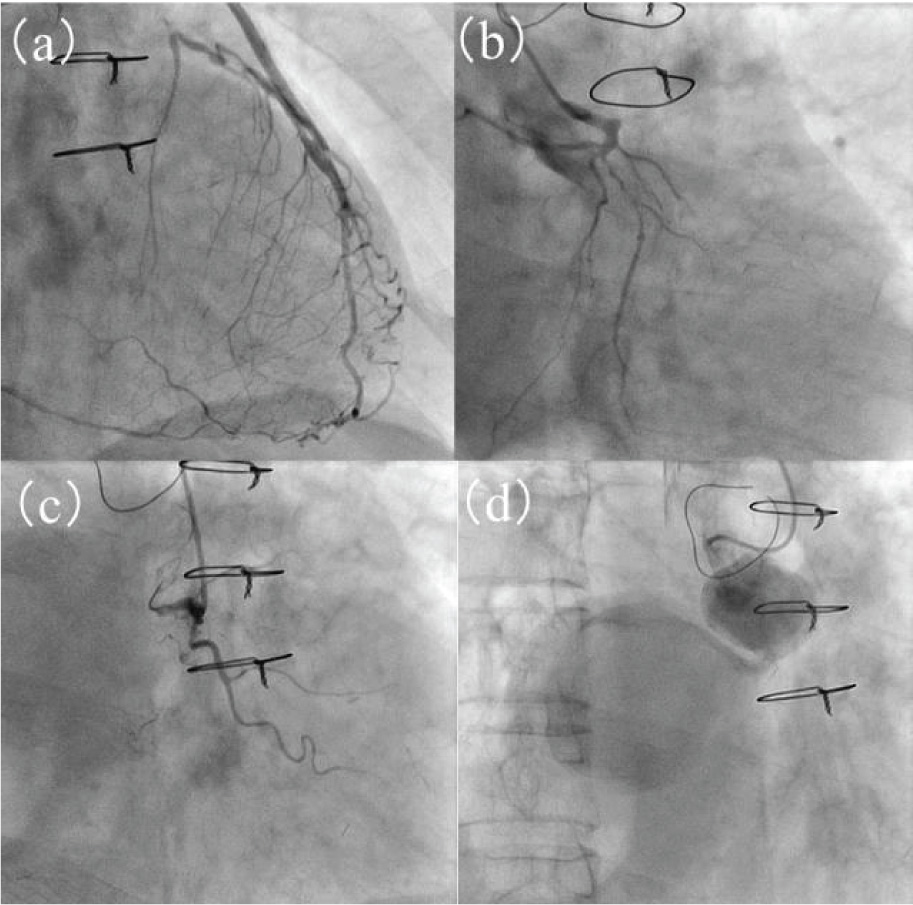
Coronary angiography.
(a, b, c) Coronary angiography was performed at the presentation of acute coronary syndrome, revealing that the proximal left anterior descending artery was totally occluded and the left circumflex artery and right carotid artery (RCA) were severely stenosed. (d) Small and large graft aneurysms were visible in the saphenous vein graft of the RCA.
Four years later, echocardiography revealed a giant mass in the right atrium. Coronary CT angiography showed that the giant aneurysm had grown to 52.1 by 63.8 mm and revealed a second, smaller aneurysm (Figures 2b, 4). Blood flowed lightly through the small lumen of the large aneurysm.
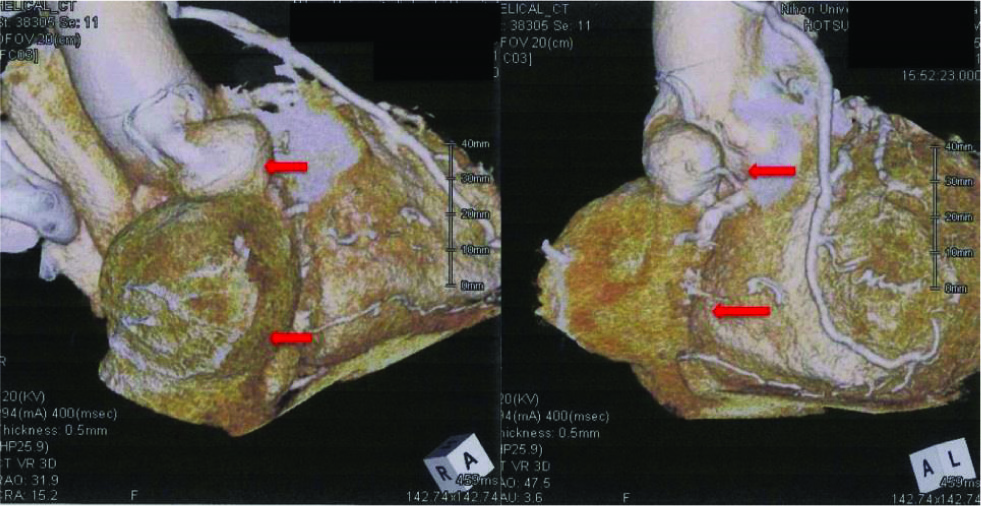
ein graft aneurysm on admission in 3D computed tomography (volume rendering image).
Saphenous vein graft aneurysms with diameters of 27 mm and 64 mm, respectively, were found from the head side position in front of the right atrium (red arrows).
The SVGA was resected to reduce the risk of rupture (Figure 5) and was diagnosed as a true aneurysm pathologically (Figure 6). The patient was discharged without postoperative complications.
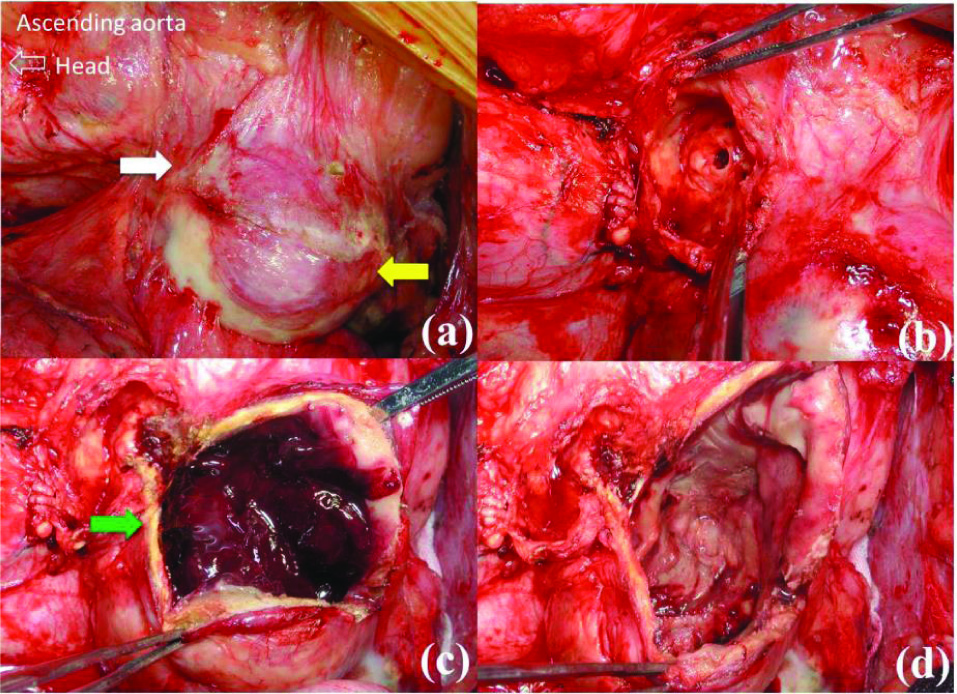
Aneurysm resection.
Proximal small vein aneurysm near the proximal anastomosis (white arrow) and large aneurysm anterior to the right atrium (yellow arrow).
Lumen within the incised proximal aneurysm.
A large amount of fresh thrombi in the distal aneurysm (green arrow).
Luminal cavity within the distal aneurysm after thrombectomy.
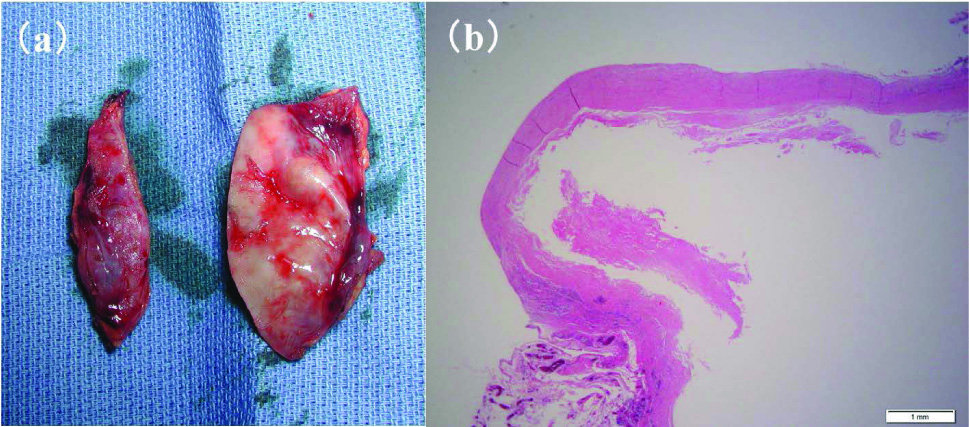
Resected vein graft aneurysm (a) and its microscopic findings (b)
The wall thickness of resected vein graft aneurysm was thinner than the healthy segment. Normal three-layer structure was observed microscopically in the enlarged segment of the resected vein graft aneurysm (hematoxylin-eosin stain).
Ethical approval: The research related to human use has complied with all the relevant national regulations and institutional policies in accordance with the tenets of the Helsinki Declaration and has been approved by the authors’ institutional review board (or equivalent) committee.
Informed consent has been obtained from all individuals included in this study.
3 Discussion
Saphenous vein graft aneurysms are rare and may be caused by atherosclerosis-like phenomena of the vein graft, weakness around the vein valve, rupturing of the suture of the graft anastomosis, or perioperative graft injury [3,4]. The cause in our case was unclear.
If the diameter of an aneurysm is less than 1 cm with adequate blood flow, medically conservative treatment is commonly indicated, with the international normalized ratio maintained at 2 to 2.5 to prevent emboli. Magnetic resonance imaging and/or CT should be required during follow-up [5]. If the aneurysm’s diameter is 2 cm or more, or is rapidly expanding, surgical intervention is recommended [6].
Some reports suggest that coil embolization or mildly invasive catheter intervention with the closure device (Amplatzer vascular plug®, Amplatzer Vascular Plug II®) can substitute for surgical treatment [7-10]. However, the success rate of the catheter intervention is not very high. It has been reported that the vein graft aneurysm is considered to be an indication for surgical treatment when the diameter of the aneurysm is more than 20 mm [11]. In our case, the graft aneurysm was more than 20 mm before the ACS developed, hence, the requirement for surgery.
The optimal management of this rare complication is not well established. The recommendation for management is as stated in our case report, rather than recommended by evidence-based practice or consensus statement.
In summary, this case suggested that aggressive treatment that includes surgical intervention should be considered before the aneurysm becomes larger, even if it is asymptomatic.
Conflict of interest statement: Authors state no conflict of interest.
References
[1] Kazui T, Harada H, Komatsu S: Saphenous vein aneurysm following coronary artery bypass grafting. J Cardiovasc Surg (Torino) 1988; 29: 364-367Search in Google Scholar
[2] Sareyyupoglu B, Schaff HV, Ucar I, et al.: Surgical treatment of saphenous vein graft aneurysms after coronary artery revascularization. Ann Thorac Surg 2009; 88: 1801-180510.1016/j.athoracsur.2009.07.048Search in Google Scholar
[3] Dabboussi M, Saade YA, Poncet A, Baehrel B: Fistula between a saphenous vein graft aneurysm and the pulmonary artery trunk. Ann Thorac Surg 2001; 71:1356-135810.1016/S0003-4975(00)01900-7Search in Google Scholar
[4] Benchimol A, Harris CL, Desser KB, Fleming H: Aneurysm of an aorto-coronary artery saphenous vein bypass graft–a case report. Vasc Surg 1975; 9: 261-26410.1177/153857447500900410Search in Google Scholar PubMed
[5] Rana O, Greaves K, Shepherd D, Parvin S, Swallow R: Saphenous vein graft aneurysm: an incidental finding. BMJ Case Rep 2009; pii: bcr07.2008.045510.1136/bcr.07.2008.0455Search in Google Scholar PubMed PubMed Central
[6] Nishimura K, Nakamura Y, Harada S, et al.: Saphenous vein graft aneurysm after coronary artery bypass grafting. Ann Thorac Cardiovasc Surg 2009; 15: 61-63Search in Google Scholar
[7] Dimitri WR, Reid AW, Dunn FG: Leaking false aneurysm of right coronary saphenous vein graft; successful treatment by percutaneous coil embolization. Br Heart J 1992; 68:61910.1136/hrt.68.12.619Search in Google Scholar PubMed PubMed Central
[8] Katoh H, Nozue T, Michishita I: A case of giant saphenous vein graft aneurysm successfully treated with catheter intervention. Catheter Cardiovasc Interv. 2015 May 26; doi: 10.1002/ccd.25984. [Epub ahead of print]10.1002/ccd.25984Search in Google Scholar PubMed PubMed Central
[9] Kim D, Guthaner DF, Wexler L: Transcatheter embolization of a leaking pseudoaneurysm of saphenous vein aortocoronary bypass graft. Cathet Cardiovasc Diagn 1983; 9: 591-59410.1002/ccd.1810090609Search in Google Scholar PubMed
[10] Ayub B, Martinez MW, Jaffe AS, Couri DM: Giant saphenous vein graft pseudoaneurysm: treatment with a vascular occlusion device. Interact Cardiovasc Thorac Surg. 2012;15(1):164-16510.1093/icvts/ivr167Search in Google Scholar PubMed PubMed Central
[11] Memon AQ, Huang RI, Marcus F et al.: Saphenous vein graft aneurysm: case report and review. Cardiol Res 2003; 11: 26-3410.1097/00045415-200301000-00006Search in Google Scholar PubMed
© 2016 Tadateru Takayama et al.
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License.
