Abstract
Background
The aim of this study was to evaluate the neuroprotective effect of surgery combined with traditional Chinese medicine(TCM)in the treatment of glaucoma by meta-analysis based on clinical controlled trial.
Methods
All the prospective randomized controlled trialsof surgery combined with TCM in the treatment of glaucoma were searched in the databases of Medline (1960-2015.1), CENTRAL (the Cochrane central register of controlled trials 1989-2015.1, EMBASE (1980∼2015.1) and CNKI (1979-2015.1). Two reviewers independently assessed the quality of the included studies, extracted the relevant data and performed a cross-check. The pooled relative risk (RR) or standard mean difference (SMD) of surgery combined with TCM versus western medicine or surgery alone were calculated as the effect size by meta-analysis method. All the data was analyzed by stata11.0 software (http://www.stata.com; Stata Corporation, College Station, TX).
Results
Finally, eleven clinical controlledtrails with 843 subjects were included in this meta-analysis. The pooled results indicated that the surgery combined with TCM treatment procedure can significant improve the vision recovery rate compared to control group (RR=1.22, 95% CI:1.06∼1.40, P=0.005); And after treatment, the visual field in combined group was significantly improved compared to control group (SMD=0.26∼95% CI:0.09∼0.43, P=0.003).
Conclusion
Surgery combined with TCM can improve the vision recovery rate and the visual fieldin the treatment of glaucoma compared to surgery or western medicine alone.
1 Introduction
Glaucoma is a term for a group of eye disorders which result in damage to the optic nerve [1]. Most of the damage to the optic nerve is related to elevated intraocular pressure (IOP) [2]. Glaucoma is the most commonly diagnosed eye disease, considered as the leading cause of blindness world-wide [3]. The exact pathogenesis for glaucoma is still not clear. Epidemiological data indicates that glaucoma may be associated with genetic susceptibility, mood swings, fatigue and other factors [4]. The goals of glaucoma management are to avoid nerve damage and preserve visual field and total quality of life for patients with minimal side effects. At present, laser surgery, conventional surgery and medicine are used to treat glaucoma. Recently, several clinical studies reported that clinical efficacy can be improved by surgery combined with traditional Chinese medicine (TCM) in the treatment of glaucoma [5, 6]. However, the effectiveness of the combined treatment varied considerably among the published studies with small sample sizes. Accordingly, we performed a meta-analysis on the basis of published clinical trials in order to identify whether the combined treatment was superior to surgery alone.
2 Materials and methods
2.1 Studies identification
Clinical controlled trials comparing surgery plus TCM vs. surgery or surgery plus western medicine for the treatment of glaucoma, published before January 2015, were identified through an electronic sensitive search of Medline, the Cochrane central register of controlled trials, EMBSE and CNKI databases. The searching term was glaucoma [MeSH]/glaucoma [text]; Chinese medical[MeSH]/Chinese medical[test]; Chinese medicine [MeSH]/Chinese medicine[test]. And the corresponding free text words were also used as the searching term. The title and abstract of identified studies were firstly evaluated to assess whether it was appropriate to the inclusion criteria or not. Following this, all of the potentially relevant trials were evaluated in full-text paper and all references of included articles were further scanned for additional analysis.
2.2 Inclusion Criteria
The patient inclusion criteria, treatment methods and outcomes for each individual study were extracted and checked by (LC) as described by the Cochrane Handbook formeta-analysis of randomized controlled trials [7]. The inclusion for this meta-analysis was as follows: (1) The patients included in each individual study were diagnosed of glaucoma with no restriction of age and gender. (2) The treatment was surgery+TMC in the experiment group and surgery alone or surgery+western medicine in the control group. (3) The outcomes were vision recovery rate and visual field improvement. The study design was prospective clinical trials without restriction of randomization.
2.3 Data Extraction
All the data for each individual study was extracted by two reviewers independently. If disagreement was found, the third investigator was consulted for consensus. The general information (name of the first author, year of publication, number of patients, treatment methods), for each included study was extracted. The outcome data of vision recovery and visual field were recorded for each individual studies.
2.4 Statistical analysis
STATA/SE 11.0 (Stata Corp LP, http://www.stata.com) was used to perform the statistical analysis. Dichotomous data is calculated as the risk ratio (RR) with a95% confidence interval (CI). Measurement data was demonstrated by mean with its standard difference and pooled by standard mean difference (SMD). Statistical heterogeneity of the results across the included studies was evaluated by Chi-square (χ2) test [8], and the inconsistency was calculated by I2 [9]. If heterogeneity was found (χ2, p<0.05 or I2>50%), the random-effect method (Dersimonian-Laird method) was used to pool the data. Otherwise, without significant heterogeneity, fixed-effect method was used. The Egger’s tests were performed to evaluate publication bias as described by Egger [10].
3 Results
3.1 General characteristic of included studies
Through searching the electronic databases of Medline (1960∼2015.1), CENTRAL (the Cochrane central register of controlled trials 1989∼2015.1), EMBASE (1980∼2015.1) and CNKI (1979∼2015.1), a total of 113 articles were initially identified. Of these, 66 potential applicable studies, published from 2004 and 2014, were reviewed in full-text paper. Finally, 11 clinical studies [5, 6, 11-19] with 457 cases in the surgery+TCM and 386 subjects in the control group were included in this meta-analysis (Figure 1). The general information for the included studies was demonstrated in Table 1.
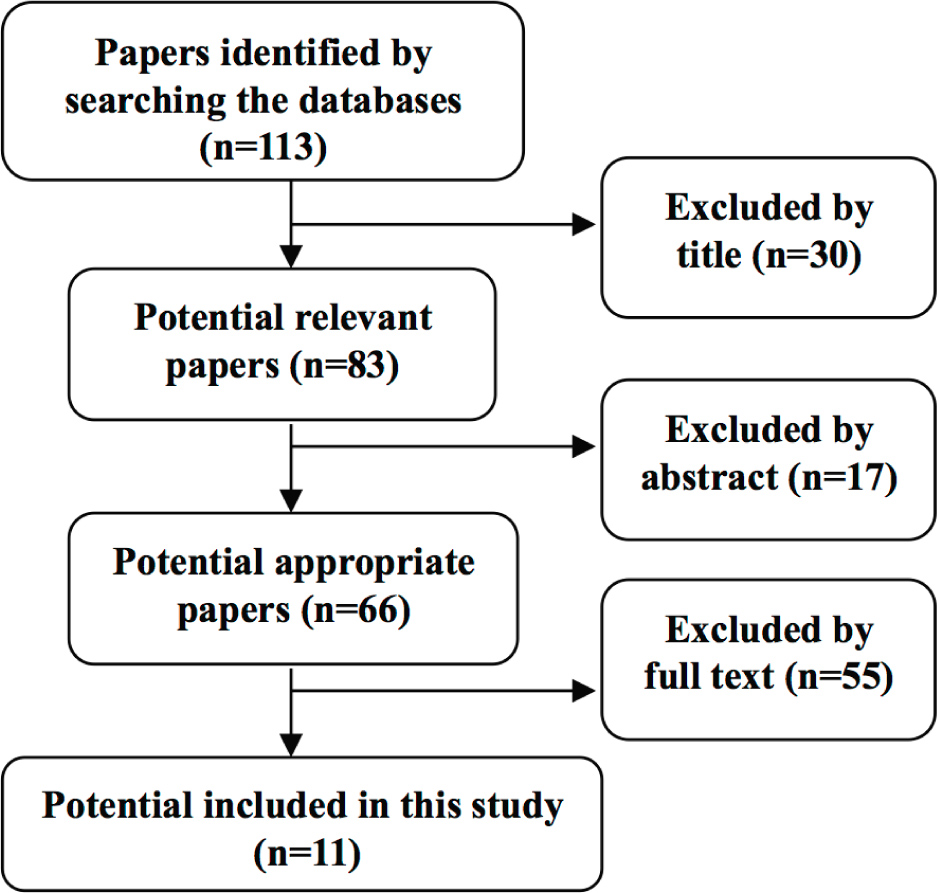
The searching flow chart of this meta-analysis
3.2 Heterogeneity assess
Significant heterogeneity was not found in the effect size of RR (I2=0.00% P = 0.647), which indicated the pooled RR was calculated by fixed effect model. For SMD, no statistical heterogeneity existed in this meta-analysis (I2=39.6% P=0.142) which indicated the SMD was pooled by fixed effect model.
The general characteristics of included studies
| First author | Year | Surgery+TCM | Surgery | Treatment (month) | ||
|---|---|---|---|---|---|---|
| n | Treatment | n | Treatment | |||
| Liu An | 2006 | 33 | Surgery+TCM | 31 | Surgery+medicine | 3 |
| Tao Rongsan | 2010 | 40 | Surgery+TCM | 38 | Surgery | 3 |
| Lin Xiaodong | 2005 | 30 | Surgery+TCM | 30 | Surgery | 3 |
| Wang Yan | 2010 | 53 | Surgery+TCM | 48 | Surgery | 3 |
| He Yuhong | 2008 | 29 | Surgery+TCM | 23 | Surgery | 4 |
| LiXiang | 2010 | 95 | Surgery+TCM | 100 | Surgery | 3 |
| Pang Youhui | 2009 | 82 | Surgery+TCM | 28 | Surgery | 3 |
| Li Jinshan | 2009 | 34 | Surgery+TCM | 28 | Surgery | 2 |
| Ye Changhua | 2003 | 23 | Surgery+TCM | 22 | Surgery+Placebo | 6 |
| Liu Dongjing | 2004 | 18 | Surgery+TCM | 18 | Surgery+Placebo | 6 |
| Xiang Minhong | 2006 | 20 | Surgery+TCM | 20 | Surgery+Placebo | 6 |
3.3 Vision recovery
Nine studies reported the vision recovery rate. The pooled results indicated that the surgery combined with traditional Chinesemedicine treatment procedure can significantly improve the vision recovery rate compared to control group (RR=1.22, 95% CI:1.06∼1.40, P=0.005), Figure 2.
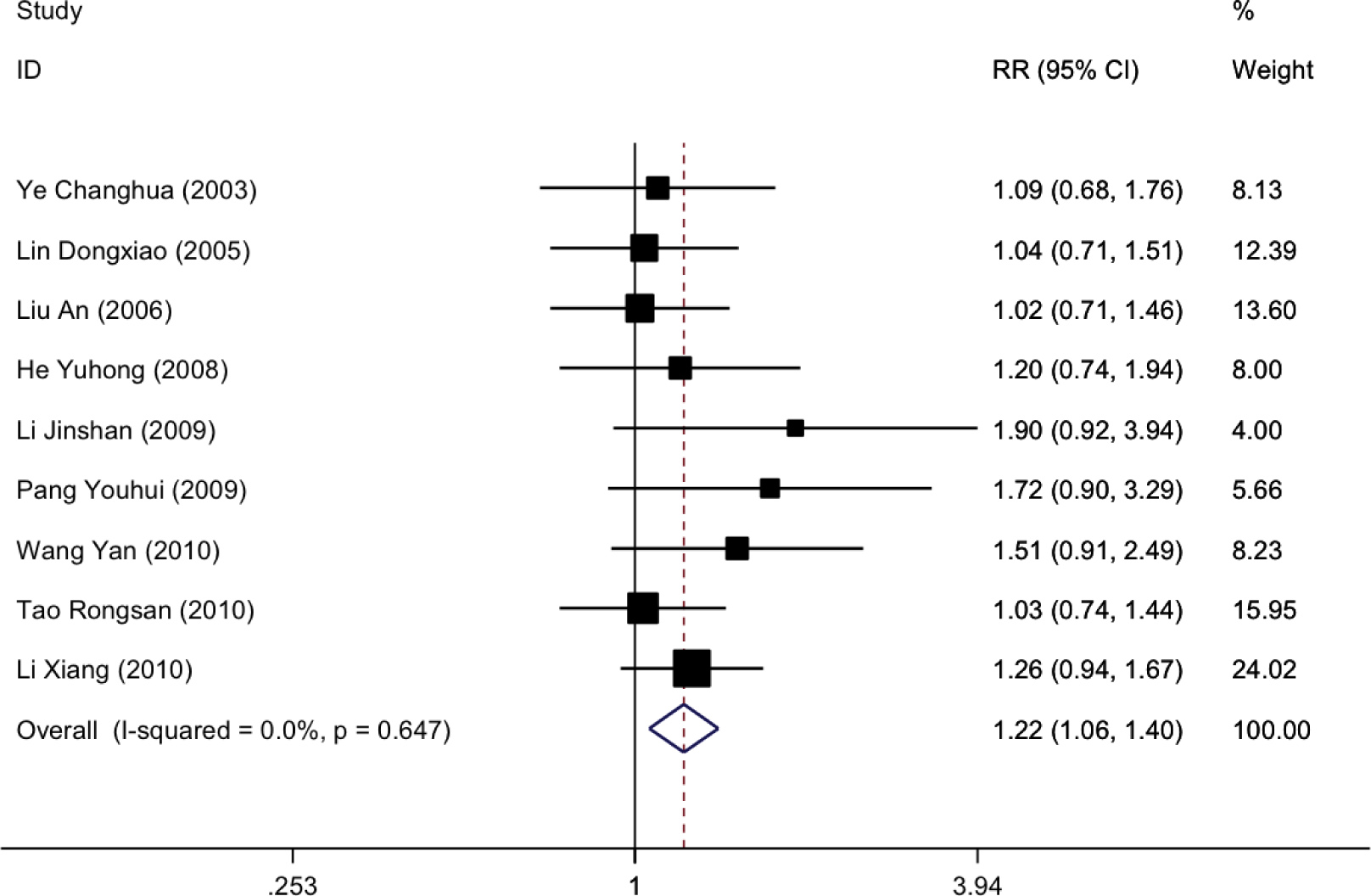
The forest plot of vision recovery treated by surgery+TCM versus surgery or western medicine alone
3.4 Visual field
Six papers reported the data of visual field improvement. The pooled results indicated that the visual field in combined group was significantly improved compared to control group (SMD=0.26, 95% CI:0.09∼0.43, P=0.003), Figure 3.
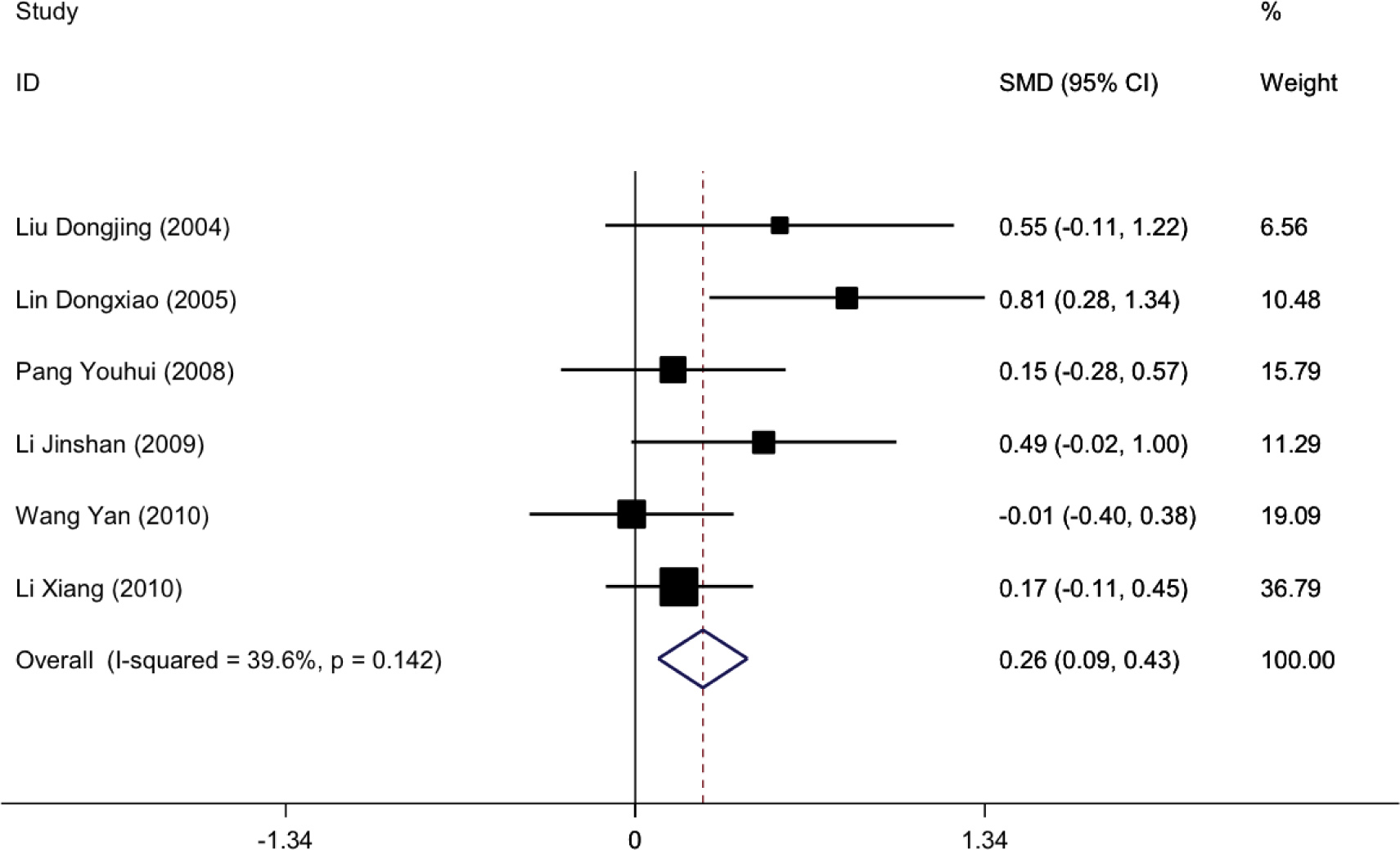
The forest plot of vision field improvement treated by surgery+TCM versus surgery or western medicine alone
3.5 Publication bias evaluation
A Begg’s funnel plot and Egger’s test were used to evaluate the publication bias [13].For the effect size of RR, the Begg’s funnel plot showed a small amount of asymmetry at the bottom (Figure 4). But the Egger’s test demonstrated no significant publication bias (t=0.78, P=0.44). For effects size of SMD, no significant publication bias was found by Egger’s test (t=1.82,P=0.143).
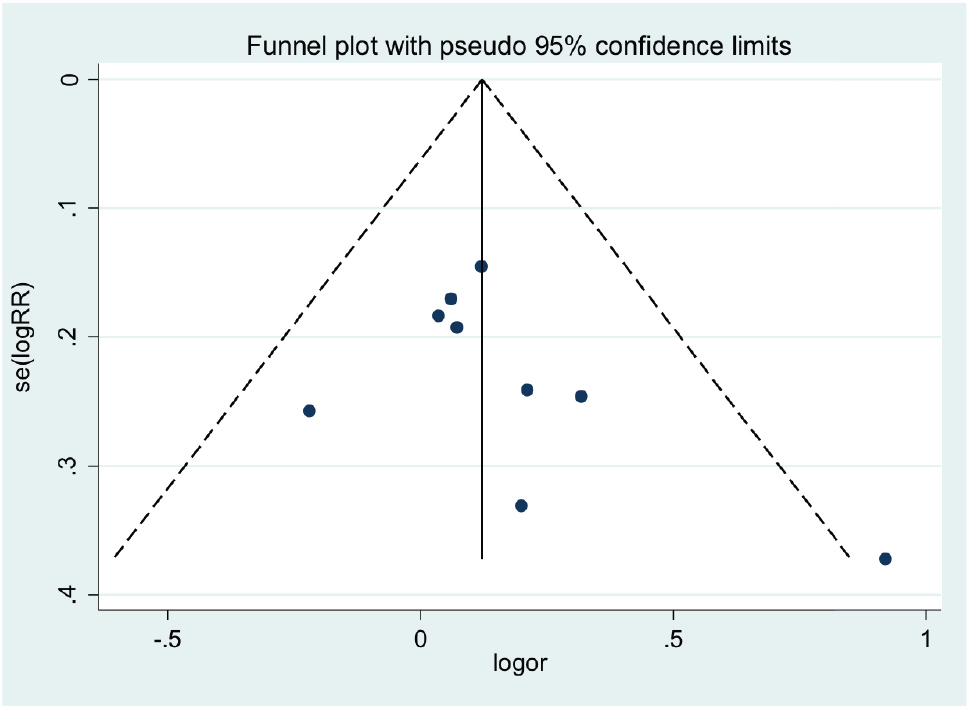
The Begg’s funnel plot in evaluation of publication bias for effect size of RR
4 Discussion
Glaucoma, the leading cause of blindness in the worldwide for people more than forty years old, is generally clinically divided into open-angle glaucoma and closed angle glaucoma. Regardless of open-angle or closed angle glaucoma, the major pathophysiology is that the intraocular pressure was increased, which can finally damage the optic nerve even leading to loss of vision.
In clinical management, the general treatment modality was to avoid or reduce nerve damage, and preserve visual field, with minimal side effects [20, 21]. At present, laser surgery, conventional surgery and medicine are commonlyused to treat glaucoma. The effectiveness of these therapies is either limited or associated with significant side effects.
Traditional Chinese medicine has a unique advantage in the treatment of chronic diseases, such as nervous system diseases. TCM believes that “the wind for glaucoma cataract” stasis caused by water, which caused the disease. The treatment should be based on supplementing Qi and nourishing Yin [22]. Several clinical studies have reported that it was effective for surgery combined with traditional Chinese medicine in the treatment of glaucoma [11-14]. But the effectiveness of the combined treatment ranged a lot among the published studies with small sample size. Thus, we searched all the published clinical studies reporting the neuroprotective effects of surgery combined with traditional Chinese medicine (TCM) in the treatment of glaucoma. We thenpooled the data by meta-analysis method. The pooled results showed that surgery combined with traditional Chinese medicine treatment procedure can significantly improve the vision recovery rate compared to control group (RR=1.33, 95% CI:1.09∼1.62, p=0.005). This means that the combined treatment modality was superior to surgery alone for vision recovery. Meta-analysis also found that the visual field in combined group was significantly improved compared to control group (SMD=0.26, 95% CI:0.09∼0.43, p=0.003).Therefore, the combined treatment had more advantages in the aspect of neuroprotective effect for patients with glaucoma.
Althoughthis meta-analysis found that surgery combined with traditional Chinese medicine can imporve the vision recovery rate and the visual field in the treatment of glaucoma compared to surgery or western medicine alone, several limitations are found in this study. Firstly, all of the 11 included studies come from China with patient ethincity “Han”, which could lead to patientselective bias. Secondly, the patient number for each included studies was relative small. Thirdly, the results were pooled by extracted data of the published paper not the individual patient data, which may lead to information bias. Fourth, the treatment period ranged from 2 months to 6 months which can lead to clinical heterogeneity. In view of the above facts,multi-center prospective randomized controlled trialsareneeded for further evaluation of the the neuroprotective effect of surgery combined with traditional chinese medicine (TCM) in the treatment of glaucoma.
Conflict of interest statement: Authors state no conflict of interest
References
[1] Song W, Huang P, Zhang C. Neuroprotective therapies for glaucoma. Drug Des Devel Ther. 2015. 9: 1469-147910.2147/DDDT.S80594Search in Google Scholar
[2] Cheng JW, Zong Y, Zeng YY, Wei RL. The prevalence of primary angle closure glaucoma in adult Asians: a systematic review and meta-analysis. PLoS One. 2014. 9(7): e10322210.1371/journal.pone.0103222Search in Google Scholar
[3] Gessesse GW, Damji KF. Advanced glaucoma: management pearls. Middle East Afr J Ophthalmol. 2013. 20(2): 131-14110.4103/0974-9233.110610Search in Google Scholar
[4] Kyari F, Abdull MM, Bastawrous A, Gilbert CE, Faal H. Epidemiology of glaucoma in sub-saharan Africa: prevalence, incidence and risk factors. Middle East Afr J Ophthalmol. 2013. 20(2): 111-12510.4103/0974-9233.110605Search in Google Scholar
[5] An L, Mingfang C, Jianwei Z. Surgery plus traditional Chines medicine for the treatment of primary closed-angle glaucoma. Journal of Shanxi College of Traditional Chinese Medicine. 2006. (06): 22-23Search in Google Scholar
[6] Rongsan T, Xiaoyuan Y, Xinxin Z, Yuzhi Q. Clinical study of late stage glaucoma treated by Integrated Chinese and Western Medicine. Henan Traditional Chinese Medicine. 2010. (10): 1004-1005Search in Google Scholar
[7] Higgins JP, Green S (2008). Cochrane Handbook for Systematic Reviews of Interventions updated March 2011 John Wiley & Sons, Available: http://www.cochrane-handbook.org/. Accessed: 2011 DEC 1210.1002/9780470712184Search in Google Scholar
[8] DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986. 7(3): 177-18810.1016/0197-2456(86)90046-2Search in Google Scholar
[9] Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003. 327(7414): 557-56010.1136/bmj.327.7414.557Search in Google Scholar PubMed PubMed Central
[10] Song F, Gilbody S. Bias in meta-analysis detected by a simple, graphical test. Increase in studies of publication bias coincided with increasing use of meta-analysis. BMJ (Clinical research ed.). 1998. 316(7129): 47110.1136/bmj.316.7129.469Search in Google Scholar
[11] Dongxiao L, Haibin Z, Gangfeng C. The protective effect of Ginkgo biloba on the visual function in patients with glaucoma. Journal of Traditional Chinese Ophthalmology. 2005. (01): 18–20Search in Google Scholar
[12] Yan W, Bo Q, Caixia Z, et al. Protective effect of Chinese medicine Yiyanmingon glaucoma optic nerve. Chinese Journal of Experimental Ophthalmology. 2010. (11): 1087-1090Search in Google Scholar
[13] Yuhong H, Ying Z. Ligustrazine combined with methylcobalamin in the treatment of postoperative glaucoma. China Medical Herald. 2008. (24): 207-210Search in Google Scholar
[14] Xiang L, Xiaoxia W, Wanjie W, Xuejun X. Qijudihuangwan and Fufangdanshen combined Mecobalamin Tablets in the treatment of glaucoma after intraocular pressure control. Shaanxi Journal of Traditional Chinese Medicine. 2010. (04): 455-457Search in Google Scholar
[15] Youhui P, He S. The effect of three kinds of traditional Chinese herbal medicine on the protection of the optic nerve in patients with glaucoma. Information on Traditional Chinese Medicine. 2008. (02): 30-32Search in Google Scholar
[16] Jinsshan L. The clinical study of Chinese herbal medicine on the protection of the optic nerve in the primary angle closure glaucoma. Northwest Pharmaceutical Journal. 2009. (05): 401-402 Search in Google Scholar
[17] Changhua Y, Youqin J. Clinical study of the protective effect of breviscapine on glaucoma nerve. Chinese Journal of Experimental Ophthalmology. 2003. (03): 307-311Search in Google Scholar
[18] Dongjing L, Xiaoming C, Chunshen L, Jing L. Optic nerve protective effect of breviscapine on glaucoma: A prospective clinical trial. Chinese Journal of Practical Ophthalmology. 2004.(04): 260-262Search in Google Scholar
[19] Hongmin X, Yisheng Z, Xingru Z. The vision field protective effects of fleabane in patients with intraocular pressure controled glaucoma. International Journal of Ophthalmology. 2006. (04): 806-809Search in Google Scholar
[20] Noecker RJ. The management of glaucoma and intraocular hypertension: current approaches and recent advances. Ther Clin Risk Manag. 2006. 2(2): 193-20610.2147/tcrm.2006.2.2.193Search in Google Scholar PubMed PubMed Central
[21] Parikh RS, Parikh SR, Navin S, Arun E, Thomas R. Practical approach to medical management of glaucoma. Indian J Ophthalmol. 2008. 56(3): 223-23010.4103/0301-4738.40362Search in Google Scholar PubMed PubMed Central
[22] Mi XS, Zhong JX, Chang RC, So KF. Research advances on the usage of traditional Chinese medicine for neuroprotection in glaucoma. J Integr Med. 2013. 11(4): 233-24010.3736/jintegrmed2013037Search in Google Scholar PubMed
© 2016 Li Chao et al.
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License.
