US9089478B2 - Peripherally administered viscous formulations - Google Patents
Peripherally administered viscous formulations Download PDFInfo
- Publication number
- US9089478B2 US9089478B2 US14/463,337 US201414463337A US9089478B2 US 9089478 B2 US9089478 B2 US 9089478B2 US 201414463337 A US201414463337 A US 201414463337A US 9089478 B2 US9089478 B2 US 9089478B2
- Authority
- US
- United States
- Prior art keywords
- triamcinolone
- peripheral
- particles
- cps
- formulation
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Expired - Lifetime
Links
- 239000000203 mixture Substances 0.000 title claims abstract description 356
- 238000009472 formulation Methods 0.000 title claims abstract description 177
- 239000002245 particle Substances 0.000 claims abstract description 142
- 229960005294 triamcinolone Drugs 0.000 claims abstract description 90
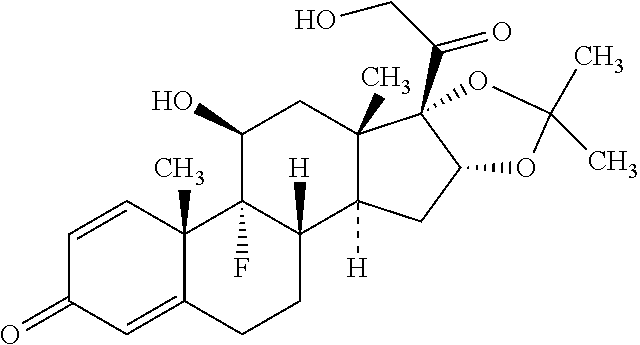
- GFNANZIMVAIWHM-OBYCQNJPSA-N triamcinolone Chemical compound O=C1C=C[C@]2(C)[C@@]3(F)[C@@H](O)C[C@](C)([C@@]([C@H](O)C4)(O)C(=O)CO)[C@@H]4[C@@H]3CCC2=C1 GFNANZIMVAIWHM-OBYCQNJPSA-N 0.000 claims abstract description 90
- 238000002347 injection Methods 0.000 claims abstract description 78
- 239000007924 injection Substances 0.000 claims abstract description 78
- 238000000034 method Methods 0.000 claims abstract description 54
- YNDXUCZADRHECN-JNQJZLCISA-N triamcinolone acetonide Chemical group C1CC2=CC(=O)C=C[C@]2(C)[C@]2(F)[C@@H]1[C@@H]1C[C@H]3OC(C)(C)O[C@@]3(C(=O)CO)[C@@]1(C)C[C@@H]2O YNDXUCZADRHECN-JNQJZLCISA-N 0.000 claims description 114
- 229920002674 hyaluronan Polymers 0.000 claims description 90
- 229960003160 hyaluronic acid Drugs 0.000 claims description 78
- KIUKXJAPPMFGSW-DNGZLQJQSA-N (2S,3S,4S,5R,6R)-6-[(2S,3R,4R,5S,6R)-3-Acetamido-2-[(2S,3S,4R,5R,6R)-6-[(2R,3R,4R,5S,6R)-3-acetamido-2,5-dihydroxy-6-(hydroxymethyl)oxan-4-yl]oxy-2-carboxy-4,5-dihydroxyoxan-3-yl]oxy-5-hydroxy-6-(hydroxymethyl)oxan-4-yl]oxy-3,4,5-trihydroxyoxane-2-carboxylic acid Chemical compound CC(=O)N[C@H]1[C@H](O)O[C@H](CO)[C@@H](O)[C@@H]1O[C@H]1[C@H](O)[C@@H](O)[C@H](O[C@H]2[C@@H]([C@@H](O[C@H]3[C@@H]([C@@H](O)[C@H](O)[C@H](O3)C(O)=O)O)[C@H](O)[C@@H](CO)O2)NC(C)=O)[C@@H](C(O)=O)O1 KIUKXJAPPMFGSW-DNGZLQJQSA-N 0.000 claims description 77
- 229960002117 triamcinolone acetonide Drugs 0.000 claims description 60
- WCDDVEOXEIYWFB-VXORFPGASA-N (2s,3s,4r,5r,6r)-3-[(2s,3r,5s,6r)-3-acetamido-5-hydroxy-6-(hydroxymethyl)oxan-2-yl]oxy-4,5,6-trihydroxyoxane-2-carboxylic acid Chemical compound CC(=O)N[C@@H]1C[C@H](O)[C@@H](CO)O[C@H]1O[C@@H]1[C@@H](C(O)=O)O[C@@H](O)[C@H](O)[C@H]1O WCDDVEOXEIYWFB-VXORFPGASA-N 0.000 claims description 36
- 229940014041 hyaluronate Drugs 0.000 claims description 36
- 239000011159 matrix material Substances 0.000 claims description 15
- 229920000858 Cyclodextrin Polymers 0.000 claims description 10
- 201000002661 Spondylitis Diseases 0.000 claims description 7
- 206010041591 Spinal osteoarthritis Diseases 0.000 claims description 6
- 208000005801 spondylosis Diseases 0.000 claims description 6
- TZIZWYVVGLXXFV-FLRHRWPCSA-N Triamcinolone hexacetonide Chemical group C1CC2=CC(=O)C=C[C@]2(C)[C@]2(F)[C@@H]1[C@@H]1C[C@H]3OC(C)(C)O[C@@]3(C(=O)COC(=O)CC(C)(C)C)[C@@]1(C)C[C@@H]2O TZIZWYVVGLXXFV-FLRHRWPCSA-N 0.000 claims description 5
- WHGYBXFWUBPSRW-FOUAGVGXSA-N beta-cyclodextrin Chemical compound OC[C@H]([C@H]([C@@H]([C@H]1O)O)O[C@H]2O[C@@H]([C@@H](O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O3)[C@H](O)[C@H]2O)CO)O[C@@H]1O[C@H]1[C@H](O)[C@@H](O)[C@@H]3O[C@@H]1CO WHGYBXFWUBPSRW-FOUAGVGXSA-N 0.000 claims description 5
- 206010037779 Radiculopathy Diseases 0.000 claims description 4
- 229960004853 betadex Drugs 0.000 claims description 4
- 229960004221 triamcinolone hexacetonide Drugs 0.000 claims description 4
- 239000001116 FEMA 4028 Substances 0.000 claims description 3
- 235000011175 beta-cyclodextrine Nutrition 0.000 claims description 3
- HFHDHCJBZVLPGP-UHFFFAOYSA-N schardinger α-dextrin Chemical compound O1C(C(C2O)O)C(CO)OC2OC(C(C2O)O)C(CO)OC2OC(C(C2O)O)C(CO)OC2OC(C(O)C2O)C(CO)OC2OC(C(C2O)O)C(CO)OC2OC2C(O)C(O)C1OC2CO HFHDHCJBZVLPGP-UHFFFAOYSA-N 0.000 claims description 3
- 229940097346 sulfobutylether-beta-cyclodextrin Drugs 0.000 claims description 3
- 230000002093 peripheral effect Effects 0.000 abstract description 154
- 230000001939 inductive effect Effects 0.000 abstract description 35
- 238000007918 intramuscular administration Methods 0.000 abstract description 14
- 239000008365 aqueous carrier Substances 0.000 abstract description 8
- 239000003246 corticosteroid Substances 0.000 description 97
- 239000008194 pharmaceutical composition Substances 0.000 description 53
- 239000000725 suspension Substances 0.000 description 49
- FAPWRFPIFSIZLT-UHFFFAOYSA-M Sodium chloride Chemical compound [Na+].[Cl-] FAPWRFPIFSIZLT-UHFFFAOYSA-M 0.000 description 47
- XLYOFNOQVPJJNP-UHFFFAOYSA-N water Substances O XLYOFNOQVPJJNP-UHFFFAOYSA-N 0.000 description 39
- 229940079593 drug Drugs 0.000 description 38
- 239000003814 drug Substances 0.000 description 38
- 150000003431 steroids Chemical class 0.000 description 38
- YWIVKILSMZOHHF-QJZPQSOGSA-N sodium;(2s,3s,4s,5r,6r)-6-[(2s,3r,4r,5s,6r)-3-acetamido-2-[(2s,3s,4r,5r,6r)-6-[(2r,3r,4r,5s,6r)-3-acetamido-2,5-dihydroxy-6-(hydroxymethyl)oxan-4-yl]oxy-2-carboxy-4,5-dihydroxyoxan-3-yl]oxy-5-hydroxy-6-(hydroxymethyl)oxan-4-yl]oxy-3,4,5-trihydroxyoxane-2- Chemical compound [Na+].CC(=O)N[C@H]1[C@H](O)O[C@H](CO)[C@@H](O)[C@@H]1O[C@H]1[C@H](O)[C@@H](O)[C@H](O[C@H]2[C@@H]([C@@H](O[C@H]3[C@@H]([C@@H](O)[C@H](O)[C@H](O3)C(O)=O)O)[C@H](O)[C@@H](CO)O2)NC(C)=O)[C@@H](C(O)=O)O1 YWIVKILSMZOHHF-QJZPQSOGSA-N 0.000 description 29
- 229920002385 Sodium hyaluronate Polymers 0.000 description 28
- 235000002639 sodium chloride Nutrition 0.000 description 26
- 229940010747 sodium hyaluronate Drugs 0.000 description 26
- 230000004054 inflammatory process Effects 0.000 description 25
- 239000011780 sodium chloride Substances 0.000 description 25
- 206010061218 Inflammation Diseases 0.000 description 24
- 239000003755 preservative agent Substances 0.000 description 24
- 229910001868 water Inorganic materials 0.000 description 24
- 210000002540 macrophage Anatomy 0.000 description 22
- WVDDGKGOMKODPV-UHFFFAOYSA-N Benzyl alcohol Chemical compound OCC1=CC=CC=C1 WVDDGKGOMKODPV-UHFFFAOYSA-N 0.000 description 21
- 239000013078 crystal Substances 0.000 description 21
- 239000000499 gel Substances 0.000 description 21
- 229920000642 polymer Polymers 0.000 description 20
- 210000001519 tissue Anatomy 0.000 description 20
- 206010003246 arthritis Diseases 0.000 description 19
- 230000001225 therapeutic effect Effects 0.000 description 19
- 239000013543 active substance Substances 0.000 description 17
- 201000008482 osteoarthritis Diseases 0.000 description 17
- 238000013268 sustained release Methods 0.000 description 15
- 239000012730 sustained-release form Substances 0.000 description 15
- 230000008901 benefit Effects 0.000 description 14
- 230000000694 effects Effects 0.000 description 14
- 230000002335 preservative effect Effects 0.000 description 14
- RYFMWSXOAZQYPI-UHFFFAOYSA-K trisodium phosphate Chemical compound [Na+].[Na+].[Na+].[O-]P([O-])([O-])=O RYFMWSXOAZQYPI-UHFFFAOYSA-K 0.000 description 14
- 239000008215 water for injection Substances 0.000 description 14
- 229940063199 kenalog Drugs 0.000 description 13
- 238000012545 processing Methods 0.000 description 12
- 230000002829 reductive effect Effects 0.000 description 12
- 229910000162 sodium phosphate Inorganic materials 0.000 description 12
- 239000001488 sodium phosphate Substances 0.000 description 12
- 235000011008 sodium phosphates Nutrition 0.000 description 12
- 230000001965 increasing effect Effects 0.000 description 10
- 230000003110 anti-inflammatory effect Effects 0.000 description 9
- 208000037265 diseases, disorders, signs and symptoms Diseases 0.000 description 9
- 239000006185 dispersion Substances 0.000 description 9
- 230000002500 effect on skin Effects 0.000 description 9
- 239000000843 powder Substances 0.000 description 9
- 239000000243 solution Substances 0.000 description 9
- 239000000872 buffer Substances 0.000 description 8
- 201000010099 disease Diseases 0.000 description 8
- 230000002757 inflammatory effect Effects 0.000 description 8
- 230000007170 pathology Effects 0.000 description 8
- 235000019445 benzyl alcohol Nutrition 0.000 description 7
- 229960001334 corticosteroids Drugs 0.000 description 7
- 229940061607 dibasic sodium phosphate Drugs 0.000 description 7
- BNIILDVGGAEEIG-UHFFFAOYSA-L disodium hydrogen phosphate Chemical compound [Na+].[Na+].OP([O-])([O-])=O BNIILDVGGAEEIG-UHFFFAOYSA-L 0.000 description 7
- 239000000017 hydrogel Substances 0.000 description 7
- 239000007943 implant Substances 0.000 description 7
- 230000028709 inflammatory response Effects 0.000 description 7
- 239000004615 ingredient Substances 0.000 description 7
- 238000002156 mixing Methods 0.000 description 7
- 229940045641 monobasic sodium phosphate Drugs 0.000 description 7
- 229910000403 monosodium phosphate Inorganic materials 0.000 description 7
- 235000019799 monosodium phosphate Nutrition 0.000 description 7
- 210000003205 muscle Anatomy 0.000 description 7
- 230000002035 prolonged effect Effects 0.000 description 7
- AJPJDKMHJJGVTQ-UHFFFAOYSA-M sodium dihydrogen phosphate Chemical compound [Na+].OP(O)([O-])=O AJPJDKMHJJGVTQ-UHFFFAOYSA-M 0.000 description 7
- 239000000126 substance Substances 0.000 description 7
- 241001465754 Metazoa Species 0.000 description 6
- 206010069093 Non-infectious endophthalmitis Diseases 0.000 description 6
- GVJHHUAWPYXKBD-UHFFFAOYSA-N d-alpha-tocopherol Natural products OC1=C(C)C(C)=C2OC(CCCC(C)CCCC(C)CCCC(C)C)(C)CCC2=C1C GVJHHUAWPYXKBD-UHFFFAOYSA-N 0.000 description 6
- 238000009826 distribution Methods 0.000 description 6
- 210000001503 joint Anatomy 0.000 description 6
- 208000018937 joint inflammation Diseases 0.000 description 6
- 230000000670 limiting effect Effects 0.000 description 6
- 238000004519 manufacturing process Methods 0.000 description 6
- 238000003860 storage Methods 0.000 description 6
- 231100000331 toxic Toxicity 0.000 description 6
- 108030001720 Bontoxilysin Proteins 0.000 description 5
- 206010066366 Toxic anterior segment syndrome Diseases 0.000 description 5
- 229930003427 Vitamin E Natural products 0.000 description 5
- 230000002776 aggregation Effects 0.000 description 5
- 229940053031 botulinum toxin Drugs 0.000 description 5
- 230000007423 decrease Effects 0.000 description 5
- 238000009792 diffusion process Methods 0.000 description 5
- 238000004090 dissolution Methods 0.000 description 5
- WIGCFUFOHFEKBI-UHFFFAOYSA-N gamma-tocopherol Natural products CC(C)CCCC(C)CCCC(C)CCCC1CCC2C(C)C(O)C(C)C(C)C2O1 WIGCFUFOHFEKBI-UHFFFAOYSA-N 0.000 description 5
- 150000004688 heptahydrates Chemical class 0.000 description 5
- 239000000463 material Substances 0.000 description 5
- 150000004682 monohydrates Chemical class 0.000 description 5
- 239000000546 pharmaceutical excipient Substances 0.000 description 5
- 230000008569 process Effects 0.000 description 5
- 229960002668 sodium chloride Drugs 0.000 description 5
- 239000004094 surface-active agent Substances 0.000 description 5
- 208000024891 symptom Diseases 0.000 description 5
- 201000004595 synovitis Diseases 0.000 description 5
- 230000002588 toxic effect Effects 0.000 description 5
- 229940046009 vitamin E Drugs 0.000 description 5
- 235000019165 vitamin E Nutrition 0.000 description 5
- 239000011709 vitamin E Substances 0.000 description 5
- 208000006820 Arthralgia Diseases 0.000 description 4
- 238000012371 Aseptic Filling Methods 0.000 description 4
- 102000004127 Cytokines Human genes 0.000 description 4
- 108090000695 Cytokines Proteins 0.000 description 4
- 230000004913 activation Effects 0.000 description 4
- 238000005054 agglomeration Methods 0.000 description 4
- 238000006243 chemical reaction Methods 0.000 description 4
- 239000012141 concentrate Substances 0.000 description 4
- 238000013265 extended release Methods 0.000 description 4
- 230000001815 facial effect Effects 0.000 description 4
- 239000000945 filler Substances 0.000 description 4
- 239000011521 glass Substances 0.000 description 4
- KIUKXJAPPMFGSW-MNSSHETKSA-N hyaluronan Chemical compound CC(=O)N[C@H]1[C@H](O)O[C@H](CO)[C@@H](O)C1O[C@H]1[C@H](O)[C@@H](O)[C@H](O[C@H]2[C@@H](C(O[C@H]3[C@@H]([C@@H](O)[C@H](O)[C@H](O3)C(O)=O)O)[C@H](O)[C@@H](CO)O2)NC(C)=O)[C@@H](C(O)=O)O1 KIUKXJAPPMFGSW-MNSSHETKSA-N 0.000 description 4
- 229940099552 hyaluronan Drugs 0.000 description 4
- 230000005847 immunogenicity Effects 0.000 description 4
- 230000000266 injurious effect Effects 0.000 description 4
- 235000010482 polyoxyethylene sorbitan monooleate Nutrition 0.000 description 4
- 239000000244 polyoxyethylene sorbitan monooleate Substances 0.000 description 4
- 229940068968 polysorbate 80 Drugs 0.000 description 4
- 229920000053 polysorbate 80 Polymers 0.000 description 4
- 239000002244 precipitate Substances 0.000 description 4
- 210000003491 skin Anatomy 0.000 description 4
- 238000007920 subcutaneous administration Methods 0.000 description 4
- 206010003694 Atrophy Diseases 0.000 description 3
- 208000008035 Back Pain Diseases 0.000 description 3
- 206010020751 Hypersensitivity Diseases 0.000 description 3
- 208000003456 Juvenile Arthritis Diseases 0.000 description 3
- 229910019142 PO4 Inorganic materials 0.000 description 3
- 208000002193 Pain Diseases 0.000 description 3
- 206010057249 Phagocytosis Diseases 0.000 description 3
- 239000002202 Polyethylene glycol Substances 0.000 description 3
- HEMHJVSKTPXQMS-UHFFFAOYSA-M Sodium hydroxide Chemical compound [OH-].[Na+] HEMHJVSKTPXQMS-UHFFFAOYSA-M 0.000 description 3
- AOBORMOPSGHCAX-UHFFFAOYSA-N Tocophersolan Chemical compound OCCOC(=O)CCC(=O)OC1=C(C)C(C)=C2OC(CCCC(C)CCCC(C)CCCC(C)C)(C)CCC2=C1C AOBORMOPSGHCAX-UHFFFAOYSA-N 0.000 description 3
- LEHOTFFKMJEONL-UHFFFAOYSA-N Uric Acid Chemical compound N1C(=O)NC(=O)C2=C1NC(=O)N2 LEHOTFFKMJEONL-UHFFFAOYSA-N 0.000 description 3
- 230000037444 atrophy Effects 0.000 description 3
- 239000002537 cosmetic Substances 0.000 description 3
- 238000004132 cross linking Methods 0.000 description 3
- 230000008030 elimination Effects 0.000 description 3
- 238000003379 elimination reaction Methods 0.000 description 3
- 239000002158 endotoxin Substances 0.000 description 3
- 238000004108 freeze drying Methods 0.000 description 3
- 238000002513 implantation Methods 0.000 description 3
- 238000003780 insertion Methods 0.000 description 3
- 230000037431 insertion Effects 0.000 description 3
- 238000010255 intramuscular injection Methods 0.000 description 3
- 239000007927 intramuscular injection Substances 0.000 description 3
- 230000001788 irregular Effects 0.000 description 3
- 238000002356 laser light scattering Methods 0.000 description 3
- 230000007774 longterm Effects 0.000 description 3
- 230000014759 maintenance of location Effects 0.000 description 3
- 230000005012 migration Effects 0.000 description 3
- 238000013508 migration Methods 0.000 description 3
- 230000008782 phagocytosis Effects 0.000 description 3
- NBIIXXVUZAFLBC-UHFFFAOYSA-K phosphate Chemical compound [O-]P([O-])([O-])=O NBIIXXVUZAFLBC-UHFFFAOYSA-K 0.000 description 3
- 239000010452 phosphate Substances 0.000 description 3
- 229920001223 polyethylene glycol Polymers 0.000 description 3
- 238000002360 preparation method Methods 0.000 description 3
- 230000000770 proinflammatory effect Effects 0.000 description 3
- 206010039073 rheumatoid arthritis Diseases 0.000 description 3
- 238000004062 sedimentation Methods 0.000 description 3
- 230000003381 solubilizing effect Effects 0.000 description 3
- 231100000419 toxicity Toxicity 0.000 description 3
- 230000001988 toxicity Effects 0.000 description 3
- 239000007966 viscous suspension Substances 0.000 description 3
- 150000003722 vitamin derivatives Chemical class 0.000 description 3
- 210000002517 zygapophyseal joint Anatomy 0.000 description 3
- IAKHMKGGTNLKSZ-INIZCTEOSA-N (S)-colchicine Chemical compound C1([C@@H](NC(C)=O)CC2)=CC(=O)C(OC)=CC=C1C1=C2C=C(OC)C(OC)=C1OC IAKHMKGGTNLKSZ-INIZCTEOSA-N 0.000 description 2
- FUFLCEKSBBHCMO-UHFFFAOYSA-N 11-dehydrocorticosterone Natural products O=C1CCC2(C)C3C(=O)CC(C)(C(CC4)C(=O)CO)C4C3CCC2=C1 FUFLCEKSBBHCMO-UHFFFAOYSA-N 0.000 description 2
- 206010008690 Chondrocalcinosis pyrophosphate Diseases 0.000 description 2
- 208000000094 Chronic Pain Diseases 0.000 description 2
- MFYSYFVPBJMHGN-ZPOLXVRWSA-N Cortisone Chemical compound O=C1CC[C@]2(C)[C@H]3C(=O)C[C@](C)([C@@](CC4)(O)C(=O)CO)[C@@H]4[C@@H]3CCC2=C1 MFYSYFVPBJMHGN-ZPOLXVRWSA-N 0.000 description 2
- MFYSYFVPBJMHGN-UHFFFAOYSA-N Cortisone Natural products O=C1CCC2(C)C3C(=O)CC(C)(C(CC4)(O)C(=O)CO)C4C3CCC2=C1 MFYSYFVPBJMHGN-UHFFFAOYSA-N 0.000 description 2
- 201000005569 Gout Diseases 0.000 description 2
- VEXZGXHMUGYJMC-UHFFFAOYSA-N Hydrochloric acid Chemical compound Cl VEXZGXHMUGYJMC-UHFFFAOYSA-N 0.000 description 2
- XQFRJNBWHJMXHO-RRKCRQDMSA-N IDUR Chemical compound C1[C@H](O)[C@@H](CO)O[C@H]1N1C(=O)NC(=O)C(I)=C1 XQFRJNBWHJMXHO-RRKCRQDMSA-N 0.000 description 2
- 206010061246 Intervertebral disc degeneration Diseases 0.000 description 2
- 206010023230 Joint stiffness Diseases 0.000 description 2
- 206010059176 Juvenile idiopathic arthritis Diseases 0.000 description 2
- 208000003947 Knee Osteoarthritis Diseases 0.000 description 2
- 229920000148 Polycarbophil calcium Polymers 0.000 description 2
- 229920002413 Polyhexanide Polymers 0.000 description 2
- WCUXLLCKKVVCTQ-UHFFFAOYSA-M Potassium chloride Chemical compound [Cl-].[K+] WCUXLLCKKVVCTQ-UHFFFAOYSA-M 0.000 description 2
- 206010059604 Radicular pain Diseases 0.000 description 2
- 241000219061 Rheum Species 0.000 description 2
- 229920002125 Sokalan® Polymers 0.000 description 2
- 208000007156 Spondylarthritis Diseases 0.000 description 2
- 239000004480 active ingredient Substances 0.000 description 2
- 230000001154 acute effect Effects 0.000 description 2
- 230000002411 adverse Effects 0.000 description 2
- 238000013019 agitation Methods 0.000 description 2
- 230000000172 allergic effect Effects 0.000 description 2
- 238000004458 analytical method Methods 0.000 description 2
- 239000007900 aqueous suspension Substances 0.000 description 2
- 206010003074 arachnoiditis Diseases 0.000 description 2
- 238000000149 argon plasma sintering Methods 0.000 description 2
- 208000006673 asthma Diseases 0.000 description 2
- 208000010668 atopic eczema Diseases 0.000 description 2
- 230000003416 augmentation Effects 0.000 description 2
- 230000004888 barrier function Effects 0.000 description 2
- 230000009286 beneficial effect Effects 0.000 description 2
- SNCZNSNPXMPCGN-UHFFFAOYSA-N butanediamide Chemical class NC(=O)CCC(N)=O SNCZNSNPXMPCGN-UHFFFAOYSA-N 0.000 description 2
- 210000000845 cartilage Anatomy 0.000 description 2
- 230000015556 catabolic process Effects 0.000 description 2
- 210000004027 cell Anatomy 0.000 description 2
- 230000030833 cell death Effects 0.000 description 2
- QBWCMBCROVPCKQ-UHFFFAOYSA-N chlorous acid Chemical compound OCl=O QBWCMBCROVPCKQ-UHFFFAOYSA-N 0.000 description 2
- 208000002849 chondrocalcinosis Diseases 0.000 description 2
- 229960004544 cortisone Drugs 0.000 description 2
- 230000006378 damage Effects 0.000 description 2
- 208000018180 degenerative disc disease Diseases 0.000 description 2
- 238000006731 degradation reaction Methods 0.000 description 2
- 230000003111 delayed effect Effects 0.000 description 2
- 230000008021 deposition Effects 0.000 description 2
- 210000004207 dermis Anatomy 0.000 description 2
- 238000001514 detection method Methods 0.000 description 2
- OSVXSBDYLRYLIG-UHFFFAOYSA-N dioxidochlorine(.) Chemical compound O=Cl=O OSVXSBDYLRYLIG-UHFFFAOYSA-N 0.000 description 2
- 238000012377 drug delivery Methods 0.000 description 2
- 238000002474 experimental method Methods 0.000 description 2
- 238000011049 filling Methods 0.000 description 2
- 238000001914 filtration Methods 0.000 description 2
- 239000012530 fluid Substances 0.000 description 2
- GDSRMADSINPKSL-HSEONFRVSA-N gamma-cyclodextrin Chemical compound OC[C@H]([C@H]([C@@H]([C@H]1O)O)O[C@H]2O[C@@H]([C@@H](O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O[C@H]3O[C@H](CO)[C@H]([C@@H]([C@H]3O)O)O3)[C@H](O)[C@H]2O)CO)O[C@@H]1O[C@H]1[C@H](O)[C@@H](O)[C@@H]3O[C@@H]1CO GDSRMADSINPKSL-HSEONFRVSA-N 0.000 description 2
- 229940080345 gamma-cyclodextrin Drugs 0.000 description 2
- 150000004676 glycans Chemical class 0.000 description 2
- JYGXADMDTFJGBT-VWUMJDOOSA-N hydrocortisone Chemical compound O=C1CC[C@]2(C)[C@H]3[C@@H](O)C[C@](C)([C@@](CC4)(O)C(=O)CO)[C@@H]4[C@@H]3CCC2=C1 JYGXADMDTFJGBT-VWUMJDOOSA-N 0.000 description 2
- 229960004716 idoxuridine Drugs 0.000 description 2
- 230000002163 immunogen Effects 0.000 description 2
- 208000021600 intervertebral disc degenerative disease Diseases 0.000 description 2
- 238000007913 intrathecal administration Methods 0.000 description 2
- 238000001990 intravenous administration Methods 0.000 description 2
- 230000007794 irritation Effects 0.000 description 2
- 210000000629 knee joint Anatomy 0.000 description 2
- 210000002414 leg Anatomy 0.000 description 2
- 230000007246 mechanism Effects 0.000 description 2
- 229910052751 metal Inorganic materials 0.000 description 2
- 239000002184 metal Substances 0.000 description 2
- 201000006417 multiple sclerosis Diseases 0.000 description 2
- 210000005036 nerve Anatomy 0.000 description 2
- 210000000440 neutrophil Anatomy 0.000 description 2
- 210000001539 phagocyte Anatomy 0.000 description 2
- 239000008363 phosphate buffer Substances 0.000 description 2
- 229950005134 polycarbophil Drugs 0.000 description 2
- 229940113116 polyethylene glycol 1000 Drugs 0.000 description 2
- 229920001282 polysaccharide Polymers 0.000 description 2
- 239000005017 polysaccharide Substances 0.000 description 2
- -1 prednesolone Chemical compound 0.000 description 2
- 239000000047 product Substances 0.000 description 2
- 239000002994 raw material Substances 0.000 description 2
- 230000002000 scavenging effect Effects 0.000 description 2
- 239000002002 slurry Substances 0.000 description 2
- 210000004872 soft tissue Anatomy 0.000 description 2
- 241000894007 species Species 0.000 description 2
- 210000000273 spinal nerve root Anatomy 0.000 description 2
- 208000001413 spine osteoarthritis Diseases 0.000 description 2
- 239000003381 stabilizer Substances 0.000 description 2
- 230000001954 sterilising effect Effects 0.000 description 2
- KDYFGRWQOYBRFD-UHFFFAOYSA-N succinic acid Chemical compound OC(=O)CCC(O)=O KDYFGRWQOYBRFD-UHFFFAOYSA-N 0.000 description 2
- 238000007910 systemic administration Methods 0.000 description 2
- 210000001835 viscera Anatomy 0.000 description 2
- 239000003932 viscosupplement Substances 0.000 description 2
- 230000037303 wrinkles Effects 0.000 description 2
- DTOUUUZOYKYHEP-UHFFFAOYSA-N 1,3-bis(2-ethylhexyl)-5-methyl-1,3-diazinan-5-amine Chemical compound CCCCC(CC)CN1CN(CC(CC)CCCC)CC(C)(N)C1 DTOUUUZOYKYHEP-UHFFFAOYSA-N 0.000 description 1
- VAZJLPXFVQHDFB-UHFFFAOYSA-N 1-(diaminomethylidene)-2-hexylguanidine Polymers CCCCCCN=C(N)N=C(N)N VAZJLPXFVQHDFB-UHFFFAOYSA-N 0.000 description 1
- JVKRKMWZYMKVTQ-UHFFFAOYSA-N 2-[4-[2-(2,3-dihydro-1H-inden-2-ylamino)pyrimidin-5-yl]pyrazol-1-yl]-N-(2-oxo-3H-1,3-benzoxazol-6-yl)acetamide Chemical compound C1C(CC2=CC=CC=C12)NC1=NC=C(C=N1)C=1C=NN(C=1)CC(=O)NC1=CC2=C(NC(O2)=O)C=C1 JVKRKMWZYMKVTQ-UHFFFAOYSA-N 0.000 description 1
- JJTUDXZGHPGLLC-IMJSIDKUSA-N 4511-42-6 Chemical compound C[C@@H]1OC(=O)[C@H](C)OC1=O JJTUDXZGHPGLLC-IMJSIDKUSA-N 0.000 description 1
- SQDAZGGFXASXDW-UHFFFAOYSA-N 5-bromo-2-(trifluoromethoxy)pyridine Chemical compound FC(F)(F)OC1=CC=C(Br)C=N1 SQDAZGGFXASXDW-UHFFFAOYSA-N 0.000 description 1
- 208000002874 Acne Vulgaris Diseases 0.000 description 1
- 206010067484 Adverse reaction Diseases 0.000 description 1
- 208000035285 Allergic Seasonal Rhinitis Diseases 0.000 description 1
- 206010002961 Aplasia Diseases 0.000 description 1
- 208000036487 Arthropathies Diseases 0.000 description 1
- 206010004485 Berylliosis Diseases 0.000 description 1
- BTBUEUYNUDRHOZ-UHFFFAOYSA-N Borate Chemical compound [O-]B([O-])[O-] BTBUEUYNUDRHOZ-UHFFFAOYSA-N 0.000 description 1
- 101710117542 Botulinum neurotoxin type A Proteins 0.000 description 1
- 206010048962 Brain oedema Diseases 0.000 description 1
- 206010006811 Bursitis Diseases 0.000 description 1
- 206010062746 Carditis Diseases 0.000 description 1
- 102000019034 Chemokines Human genes 0.000 description 1
- 108010012236 Chemokines Proteins 0.000 description 1
- GHXZTYHSJHQHIJ-UHFFFAOYSA-N Chlorhexidine Chemical compound C=1C=C(Cl)C=CC=1NC(N)=NC(N)=NCCCCCCN=C(N)N=C(N)NC1=CC=C(Cl)C=C1 GHXZTYHSJHQHIJ-UHFFFAOYSA-N 0.000 description 1
- 239000004155 Chlorine dioxide Substances 0.000 description 1
- 229920001287 Chondroitin sulfate Polymers 0.000 description 1
- 208000023355 Chronic beryllium disease Diseases 0.000 description 1
- 241001340526 Chrysoclista linneella Species 0.000 description 1
- 208000032544 Cicatrix Diseases 0.000 description 1
- 208000008448 Congenital adrenal hyperplasia Diseases 0.000 description 1
- PMATZTZNYRCHOR-CGLBZJNRSA-N Cyclosporin A Chemical compound CC[C@@H]1NC(=O)[C@H]([C@H](O)[C@H](C)C\C=C\C)N(C)C(=O)[C@H](C(C)C)N(C)C(=O)[C@H](CC(C)C)N(C)C(=O)[C@H](CC(C)C)N(C)C(=O)[C@@H](C)NC(=O)[C@H](C)NC(=O)[C@H](CC(C)C)N(C)C(=O)[C@H](C(C)C)NC(=O)[C@H](CC(C)C)N(C)C(=O)CN(C)C1=O PMATZTZNYRCHOR-CGLBZJNRSA-N 0.000 description 1
- 108010036949 Cyclosporine Proteins 0.000 description 1
- FBPFZTCFMRRESA-KVTDHHQDSA-N D-Mannitol Chemical compound OC[C@@H](O)[C@@H](O)[C@H](O)[C@H](O)CO FBPFZTCFMRRESA-KVTDHHQDSA-N 0.000 description 1
- QIEPWCSVQYUPIY-LEKSSAKUSA-N Delta(1)-progesterone Chemical compound C1CC2=CC(=O)C=C[C@]2(C)[C@@H]2[C@@H]1[C@@H]1CC[C@H](C(=O)C)[C@@]1(C)CC2 QIEPWCSVQYUPIY-LEKSSAKUSA-N 0.000 description 1
- 201000004624 Dermatitis Diseases 0.000 description 1
- 206010012441 Dermatitis bullous Diseases 0.000 description 1
- 206010012455 Dermatitis exfoliative Diseases 0.000 description 1
- 229920001353 Dextrin Polymers 0.000 description 1
- 239000004375 Dextrin Substances 0.000 description 1
- 208000006926 Discoid Lupus Erythematosus Diseases 0.000 description 1
- 206010013700 Drug hypersensitivity Diseases 0.000 description 1
- 208000017701 Endocrine disease Diseases 0.000 description 1
- 208000004232 Enteritis Diseases 0.000 description 1
- 108090000790 Enzymes Proteins 0.000 description 1
- 102000004190 Enzymes Human genes 0.000 description 1
- 201000011275 Epicondylitis Diseases 0.000 description 1
- 206010015218 Erythema multiforme Diseases 0.000 description 1
- 108010037362 Extracellular Matrix Proteins Proteins 0.000 description 1
- 102000010834 Extracellular Matrix Proteins Human genes 0.000 description 1
- 206010015995 Eyelid ptosis Diseases 0.000 description 1
- 206010063006 Facial spasm Diseases 0.000 description 1
- 108010010803 Gelatin Proteins 0.000 description 1
- 206010018634 Gouty Arthritis Diseases 0.000 description 1
- 206010019196 Head injury Diseases 0.000 description 1
- 208000004095 Hemifacial Spasm Diseases 0.000 description 1
- 241000282412 Homo Species 0.000 description 1
- 208000037147 Hypercalcaemia Diseases 0.000 description 1
- 201000002980 Hyperparathyroidism Diseases 0.000 description 1
- 208000012659 Joint disease Diseases 0.000 description 1
- 206010025323 Lymphomas Diseases 0.000 description 1
- 229930195725 Mannitol Natural products 0.000 description 1
- 108010000684 Matrix Metalloproteinases Proteins 0.000 description 1
- 102000002274 Matrix Metalloproteinases Human genes 0.000 description 1
- GZENKSODFLBBHQ-ILSZZQPISA-N Medrysone Chemical compound C([C@@]12C)CC(=O)C=C1[C@@H](C)C[C@@H]1[C@@H]2[C@@H](O)C[C@]2(C)[C@@H](C(C)=O)CC[C@H]21 GZENKSODFLBBHQ-ILSZZQPISA-N 0.000 description 1
- 201000009906 Meningitis Diseases 0.000 description 1
- FQISKWAFAHGMGT-SGJOWKDISA-M Methylprednisolone sodium succinate Chemical compound [Na+].C([C@@]12C)=CC(=O)C=C1[C@@H](C)C[C@@H]1[C@@H]2[C@@H](O)C[C@]2(C)[C@@](O)(C(=O)COC(=O)CCC([O-])=O)CC[C@H]21 FQISKWAFAHGMGT-SGJOWKDISA-M 0.000 description 1
- 208000009525 Myocarditis Diseases 0.000 description 1
- 206010029164 Nephrotic syndrome Diseases 0.000 description 1
- 206010030113 Oedema Diseases 0.000 description 1
- MKPDWECBUAZOHP-AFYJWTTESA-N Paramethasone Chemical compound C1([C@@H](F)C2)=CC(=O)C=C[C@]1(C)[C@@H]1[C@@H]2[C@@H]2C[C@@H](C)[C@@](C(=O)CO)(O)[C@@]2(C)C[C@@H]1O MKPDWECBUAZOHP-AFYJWTTESA-N 0.000 description 1
- 241000721454 Pemphigus Species 0.000 description 1
- 206010035664 Pneumonia Diseases 0.000 description 1
- 239000004372 Polyvinyl alcohol Substances 0.000 description 1
- 201000004681 Psoriasis Diseases 0.000 description 1
- 208000017442 Retinal disease Diseases 0.000 description 1
- 206010042033 Stevens-Johnson syndrome Diseases 0.000 description 1
- 231100000168 Stevens-Johnson syndrome Toxicity 0.000 description 1
- 241000194017 Streptococcus Species 0.000 description 1
- 208000004760 Tenosynovitis Diseases 0.000 description 1
- 208000031737 Tissue Adhesions Diseases 0.000 description 1
- 208000003441 Transfusion reaction Diseases 0.000 description 1
- 206010044608 Trichiniasis Diseases 0.000 description 1
- 108010057266 Type A Botulinum Toxins Proteins 0.000 description 1
- 206010047571 Visual impairment Diseases 0.000 description 1
- 108010079650 abobotulinumtoxinA Proteins 0.000 description 1
- 239000006096 absorbing agent Substances 0.000 description 1
- 230000001133 acceleration Effects 0.000 description 1
- 239000008351 acetate buffer Substances 0.000 description 1
- DPXJVFZANSGRMM-UHFFFAOYSA-N acetic acid;2,3,4,5,6-pentahydroxyhexanal;sodium Chemical compound [Na].CC(O)=O.OCC(O)C(O)C(O)C(O)C=O DPXJVFZANSGRMM-UHFFFAOYSA-N 0.000 description 1
- 239000002253 acid Substances 0.000 description 1
- 206010000496 acne Diseases 0.000 description 1
- 230000009056 active transport Effects 0.000 description 1
- 208000026816 acute arthritis Diseases 0.000 description 1
- 230000009798 acute exacerbation Effects 0.000 description 1
- 208000038016 acute inflammation Diseases 0.000 description 1
- 230000006022 acute inflammation Effects 0.000 description 1
- 239000002998 adhesive polymer Substances 0.000 description 1
- 239000003470 adrenal cortex hormone Substances 0.000 description 1
- 230000006838 adverse reaction Effects 0.000 description 1
- 238000004220 aggregation Methods 0.000 description 1
- 229910052783 alkali metal Inorganic materials 0.000 description 1
- 150000001340 alkali metals Chemical class 0.000 description 1
- 229910052784 alkaline earth metal Inorganic materials 0.000 description 1
- 150000001342 alkaline earth metals Chemical class 0.000 description 1
- 208000030961 allergic reaction Diseases 0.000 description 1
- 230000007815 allergy Effects 0.000 description 1
- 230000004075 alteration Effects 0.000 description 1
- 125000003368 amide group Chemical group 0.000 description 1
- 210000003484 anatomy Anatomy 0.000 description 1
- 208000007502 anemia Diseases 0.000 description 1
- 239000002260 anti-inflammatory agent Substances 0.000 description 1
- 230000001153 anti-wrinkle effect Effects 0.000 description 1
- 230000000890 antigenic effect Effects 0.000 description 1
- 210000001742 aqueous humor Anatomy 0.000 description 1
- 239000007864 aqueous solution Substances 0.000 description 1
- 230000002917 arthritic effect Effects 0.000 description 1
- QVGXLLKOCUKJST-UHFFFAOYSA-N atomic oxygen Chemical compound [O] QVGXLLKOCUKJST-UHFFFAOYSA-N 0.000 description 1
- 230000001580 bacterial effect Effects 0.000 description 1
- 229960000686 benzalkonium chloride Drugs 0.000 description 1
- CADWTSSKOVRVJC-UHFFFAOYSA-N benzyl(dimethyl)azanium;chloride Chemical compound [Cl-].C[NH+](C)CC1=CC=CC=C1 CADWTSSKOVRVJC-UHFFFAOYSA-N 0.000 description 1
- 229960002537 betamethasone Drugs 0.000 description 1
- UREBDLICKHMUKA-DVTGEIKXSA-N betamethasone Chemical compound C1CC2=CC(=O)C=C[C@]2(C)[C@]2(F)[C@@H]1[C@@H]1C[C@H](C)[C@@](C(=O)CO)(O)[C@@]1(C)C[C@@H]2O UREBDLICKHMUKA-DVTGEIKXSA-N 0.000 description 1
- 238000006065 biodegradation reaction Methods 0.000 description 1
- 210000000988 bone and bone Anatomy 0.000 description 1
- 229940089093 botox Drugs 0.000 description 1
- 229940094657 botulinum toxin type a Drugs 0.000 description 1
- 208000006752 brain edema Diseases 0.000 description 1
- 230000003139 buffering effect Effects 0.000 description 1
- 239000004067 bulking agent Substances 0.000 description 1
- JUNWLZAGQLJVLR-UHFFFAOYSA-J calcium diphosphate Chemical group [Ca+2].[Ca+2].[O-]P([O-])(=O)OP([O-])([O-])=O JUNWLZAGQLJVLR-UHFFFAOYSA-J 0.000 description 1
- 229940043256 calcium pyrophosphate Drugs 0.000 description 1
- 229920003123 carboxymethyl cellulose sodium Polymers 0.000 description 1
- 229940063834 carboxymethylcellulose sodium Drugs 0.000 description 1
- 239000000969 carrier Substances 0.000 description 1
- 238000012512 characterization method Methods 0.000 description 1
- 239000002561 chemical irritant Substances 0.000 description 1
- 239000003795 chemical substances by application Substances 0.000 description 1
- 229960003260 chlorhexidine Drugs 0.000 description 1
- 235000019398 chlorine dioxide Nutrition 0.000 description 1
- 229910001919 chlorite Inorganic materials 0.000 description 1
- 229910052619 chlorite group Inorganic materials 0.000 description 1
- 229940059329 chondroitin sulfate Drugs 0.000 description 1
- 230000003011 chondroprotective effect Effects 0.000 description 1
- 208000023819 chronic asthma Diseases 0.000 description 1
- 208000037976 chronic inflammation Diseases 0.000 description 1
- 230000006020 chronic inflammation Effects 0.000 description 1
- 229960001265 ciclosporin Drugs 0.000 description 1
- 239000007979 citrate buffer Substances 0.000 description 1
- 238000005352 clarification Methods 0.000 description 1
- 239000011248 coating agent Substances 0.000 description 1
- 238000000576 coating method Methods 0.000 description 1
- 229960001338 colchicine Drugs 0.000 description 1
- 206010009887 colitis Diseases 0.000 description 1
- 238000013329 compounding Methods 0.000 description 1
- 238000007596 consolidation process Methods 0.000 description 1
- 229920001577 copolymer Polymers 0.000 description 1
- 238000007428 craniotomy Methods 0.000 description 1
- 229920006037 cross link polymer Polymers 0.000 description 1
- 208000004921 cutaneous lupus erythematosus Diseases 0.000 description 1
- 229940097362 cyclodextrins Drugs 0.000 description 1
- 229930182912 cyclosporin Natural products 0.000 description 1
- 230000034994 death Effects 0.000 description 1
- 230000003247 decreasing effect Effects 0.000 description 1
- 230000007812 deficiency Effects 0.000 description 1
- 201000001981 dermatomyositis Diseases 0.000 description 1
- 239000003599 detergent Substances 0.000 description 1
- 229960003957 dexamethasone Drugs 0.000 description 1
- UREBDLICKHMUKA-CXSFZGCWSA-N dexamethasone Chemical compound C1CC2=CC(=O)C=C[C@]2(C)[C@]2(F)[C@@H]1[C@@H]1C[C@@H](C)[C@@](C(=O)CO)(O)[C@@]1(C)C[C@@H]2O UREBDLICKHMUKA-CXSFZGCWSA-N 0.000 description 1
- 235000019425 dextrin Nutrition 0.000 description 1
- 238000002405 diagnostic procedure Methods 0.000 description 1
- 229940052354 dibasic sodium phosphate heptahydrate Drugs 0.000 description 1
- 235000019821 dicalcium diphosphate Nutrition 0.000 description 1
- 238000010790 dilution Methods 0.000 description 1
- 239000012895 dilution Substances 0.000 description 1
- PYLIXCKOHOHGKQ-UHFFFAOYSA-L disodium;hydrogen phosphate;heptahydrate Chemical compound O.O.O.O.O.O.O.[Na+].[Na+].OP([O-])([O-])=O PYLIXCKOHOHGKQ-UHFFFAOYSA-L 0.000 description 1
- 208000035475 disorder Diseases 0.000 description 1
- 239000012153 distilled water Substances 0.000 description 1
- 230000004064 dysfunction Effects 0.000 description 1
- 229940098753 dysport Drugs 0.000 description 1
- 210000000624 ear auricle Anatomy 0.000 description 1
- 238000005538 encapsulation Methods 0.000 description 1
- 150000002148 esters Chemical class 0.000 description 1
- 235000010228 ethyl p-hydroxybenzoate Nutrition 0.000 description 1
- 229940085094 euflexxa Drugs 0.000 description 1
- 230000005713 exacerbation Effects 0.000 description 1
- 230000003090 exacerbative effect Effects 0.000 description 1
- 210000002744 extracellular matrix Anatomy 0.000 description 1
- 210000001145 finger joint Anatomy 0.000 description 1
- 238000005189 flocculation Methods 0.000 description 1
- 230000016615 flocculation Effects 0.000 description 1
- 229960001048 fluorometholone Drugs 0.000 description 1
- FAOZLTXFLGPHNG-KNAQIMQKSA-N fluorometholone Chemical compound C([C@@]12C)=CC(=O)C=C1[C@@H](C)C[C@@H]1[C@]2(F)[C@@H](O)C[C@]2(C)[C@@](O)(C(C)=O)CC[C@H]21 FAOZLTXFLGPHNG-KNAQIMQKSA-N 0.000 description 1
- 230000037406 food intake Effects 0.000 description 1
- 210000001061 forehead Anatomy 0.000 description 1
- 229920000159 gelatin Polymers 0.000 description 1
- 239000008273 gelatin Substances 0.000 description 1
- 235000019322 gelatine Nutrition 0.000 description 1
- 235000011852 gelatine desserts Nutrition 0.000 description 1
- 239000003862 glucocorticoid Substances 0.000 description 1
- 238000010438 heat treatment Methods 0.000 description 1
- 229960004867 hexetidine Drugs 0.000 description 1
- 239000008240 homogeneous mixture Substances 0.000 description 1
- 229940018991 hyalgan Drugs 0.000 description 1
- 229960000890 hydrocortisone Drugs 0.000 description 1
- 229940072322 hylan Drugs 0.000 description 1
- 230000000148 hypercalcaemia Effects 0.000 description 1
- 208000030915 hypercalcemia disease Diseases 0.000 description 1
- 230000001900 immune effect Effects 0.000 description 1
- 230000006872 improvement Effects 0.000 description 1
- 238000001727 in vivo Methods 0.000 description 1
- 238000011065 in-situ storage Methods 0.000 description 1
- 108010024001 incobotulinumtoxinA Proteins 0.000 description 1
- 208000021646 inflammation of heart layer Diseases 0.000 description 1
- 230000004968 inflammatory condition Effects 0.000 description 1
- 208000014674 injury Diseases 0.000 description 1
- 238000007919 intrasynovial administration Methods 0.000 description 1
- 201000002215 juvenile rheumatoid arthritis Diseases 0.000 description 1
- 238000002372 labelling Methods 0.000 description 1
- 230000002045 lasting effect Effects 0.000 description 1
- 230000003902 lesion Effects 0.000 description 1
- 231100000518 lethal Toxicity 0.000 description 1
- 230000001665 lethal effect Effects 0.000 description 1
- 208000032839 leukemia Diseases 0.000 description 1
- 239000007788 liquid Substances 0.000 description 1
- 238000011068 loading method Methods 0.000 description 1
- 229960001798 loteprednol Drugs 0.000 description 1
- YPZVAYHNBBHPTO-MXRBDKCISA-N loteprednol Chemical compound O=C1C=C[C@]2(C)[C@H]3[C@@H](O)C[C@](C)([C@@](CC4)(O)C(=O)OCCl)[C@@H]4[C@@H]3CCC2=C1 YPZVAYHNBBHPTO-MXRBDKCISA-N 0.000 description 1
- 239000000314 lubricant Substances 0.000 description 1
- 238000005461 lubrication Methods 0.000 description 1
- 206010025135 lupus erythematosus Diseases 0.000 description 1
- 210000004698 lymphocyte Anatomy 0.000 description 1
- 230000002132 lysosomal effect Effects 0.000 description 1
- 238000012423 maintenance Methods 0.000 description 1
- 238000007726 management method Methods 0.000 description 1
- 239000000594 mannitol Substances 0.000 description 1
- 235000010355 mannitol Nutrition 0.000 description 1
- KJLLKLRVCJAFRY-UHFFFAOYSA-N mebutizide Chemical compound ClC1=C(S(N)(=O)=O)C=C2S(=O)(=O)NC(C(C)C(C)CC)NC2=C1 KJLLKLRVCJAFRY-UHFFFAOYSA-N 0.000 description 1
- 229960001011 medrysone Drugs 0.000 description 1
- 125000002496 methyl group Chemical group [H]C([H])([H])* 0.000 description 1
- 235000010270 methyl p-hydroxybenzoate Nutrition 0.000 description 1
- 229960004584 methylprednisolone Drugs 0.000 description 1
- 239000004005 microsphere Substances 0.000 description 1
- 239000000178 monomer Substances 0.000 description 1
- 201000005962 mycosis fungoides Diseases 0.000 description 1
- 229940112646 myobloc Drugs 0.000 description 1
- 231100000252 nontoxic Toxicity 0.000 description 1
- 230000003000 nontoxic effect Effects 0.000 description 1
- 229940023593 orthovisc Drugs 0.000 description 1
- 230000001590 oxidative effect Effects 0.000 description 1
- 239000001301 oxygen Substances 0.000 description 1
- 229910052760 oxygen Inorganic materials 0.000 description 1
- 238000004806 packaging method and process Methods 0.000 description 1
- 229960002858 paramethasone Drugs 0.000 description 1
- WVDDGKGOMKODPV-ZQBYOMGUSA-N phenyl(114C)methanol Chemical compound O[14CH2]C1=CC=CC=C1 WVDDGKGOMKODPV-ZQBYOMGUSA-N 0.000 description 1
- 150000003013 phosphoric acid derivatives Chemical class 0.000 description 1
- 238000002464 physical blending Methods 0.000 description 1
- 229940068196 placebo Drugs 0.000 description 1
- 239000000902 placebo Substances 0.000 description 1
- 229920001983 poloxamer Polymers 0.000 description 1
- 229920002401 polyacrylamide Polymers 0.000 description 1
- 239000004584 polyacrylic acid Substances 0.000 description 1
- 229920000447 polyanionic polymer Polymers 0.000 description 1
- 239000008389 polyethoxylated castor oil Substances 0.000 description 1
- 208000005987 polymyositis Diseases 0.000 description 1
- 229920001296 polysiloxane Polymers 0.000 description 1
- 229920000136 polysorbate Polymers 0.000 description 1
- 229950008882 polysorbate Drugs 0.000 description 1
- 229920002689 polyvinyl acetate Polymers 0.000 description 1
- 239000011118 polyvinyl acetate Substances 0.000 description 1
- 229920002451 polyvinyl alcohol Polymers 0.000 description 1
- 229920000036 polyvinylpyrrolidone Polymers 0.000 description 1
- 239000001267 polyvinylpyrrolidone Substances 0.000 description 1
- 235000013855 polyvinylpyrrolidone Nutrition 0.000 description 1
- 239000001103 potassium chloride Substances 0.000 description 1
- 235000011164 potassium chloride Nutrition 0.000 description 1
- 230000001376 precipitating effect Effects 0.000 description 1
- 229960005205 prednisolone Drugs 0.000 description 1
- OIGNJSKKLXVSLS-VWUMJDOOSA-N prednisolone Chemical compound O=C1C=C[C@]2(C)[C@H]3[C@@H](O)C[C@](C)([C@@](CC4)(O)C(=O)CO)[C@@H]4[C@@H]3CCC2=C1 OIGNJSKKLXVSLS-VWUMJDOOSA-N 0.000 description 1
- 229960004618 prednisone Drugs 0.000 description 1
- XOFYZVNMUHMLCC-ZPOLXVRWSA-N prednisone Chemical compound O=C1C=C[C@]2(C)[C@H]3C(=O)C[C@](C)([C@@](CC4)(O)C(=O)CO)[C@@H]4[C@@H]3CCC2=C1 XOFYZVNMUHMLCC-ZPOLXVRWSA-N 0.000 description 1
- 201000001474 proteinuria Diseases 0.000 description 1
- 201000003004 ptosis Diseases 0.000 description 1
- 230000002685 pulmonary effect Effects 0.000 description 1
- ZAHRKKWIAAJSAO-UHFFFAOYSA-N rapamycin Natural products COCC(O)C(=C/C(C)C(=O)CC(OC(=O)C1CCCCN1C(=O)C(=O)C2(O)OC(CC(OC)C(=CC=CC=CC(C)CC(C)C(=O)C)C)CCC2C)C(C)CC3CCC(O)C(C3)OC)C ZAHRKKWIAAJSAO-UHFFFAOYSA-N 0.000 description 1
- 238000011084 recovery Methods 0.000 description 1
- 238000011160 research Methods 0.000 description 1
- 210000001525 retina Anatomy 0.000 description 1
- 206010039083 rhinitis Diseases 0.000 description 1
- 108010074523 rimabotulinumtoxinB Proteins 0.000 description 1
- 150000003839 salts Chemical class 0.000 description 1
- 201000000306 sarcoidosis Diseases 0.000 description 1
- 231100000241 scar Toxicity 0.000 description 1
- 230000037387 scars Effects 0.000 description 1
- 238000000926 separation method Methods 0.000 description 1
- 206010040400 serum sickness Diseases 0.000 description 1
- 230000035939 shock Effects 0.000 description 1
- QFJCIRLUMZQUOT-HPLJOQBZSA-N sirolimus Chemical compound C1C[C@@H](O)[C@H](OC)C[C@@H]1C[C@@H](C)[C@H]1OC(=O)[C@@H]2CCCCN2C(=O)C(=O)[C@](O)(O2)[C@H](C)CC[C@H]2C[C@H](OC)/C(C)=C/C=C/C=C/[C@@H](C)C[C@@H](C)C(=O)[C@H](OC)[C@H](O)/C(C)=C/[C@@H](C)C(=O)C1 QFJCIRLUMZQUOT-HPLJOQBZSA-N 0.000 description 1
- 229960002930 sirolimus Drugs 0.000 description 1
- BBMHARZCALWXSL-UHFFFAOYSA-M sodium dihydrogenphosphate monohydrate Chemical compound O.[Na+].OP(O)([O-])=O BBMHARZCALWXSL-UHFFFAOYSA-M 0.000 description 1
- 238000011146 sterile filtration Methods 0.000 description 1
- 238000004659 sterilization and disinfection Methods 0.000 description 1
- 210000004003 subcutaneous fat Anatomy 0.000 description 1
- 238000010254 subcutaneous injection Methods 0.000 description 1
- 239000007929 subcutaneous injection Substances 0.000 description 1
- KDYFGRWQOYBRFD-UHFFFAOYSA-L succinate(2-) Chemical compound [O-]C(=O)CCC([O-])=O KDYFGRWQOYBRFD-UHFFFAOYSA-L 0.000 description 1
- 239000001384 succinic acid Substances 0.000 description 1
- 150000003900 succinic acid esters Chemical class 0.000 description 1
- 150000005846 sugar alcohols Chemical class 0.000 description 1
- 229940053210 supartz Drugs 0.000 description 1
- 230000009469 supplementation Effects 0.000 description 1
- 210000001179 synovial fluid Anatomy 0.000 description 1
- 210000001258 synovial membrane Anatomy 0.000 description 1
- 229940036220 synvisc Drugs 0.000 description 1
- 230000009885 systemic effect Effects 0.000 description 1
- 229940037128 systemic glucocorticoids Drugs 0.000 description 1
- 201000000596 systemic lupus erythematosus Diseases 0.000 description 1
- 210000001738 temporomandibular joint Anatomy 0.000 description 1
- 229940126585 therapeutic drug Drugs 0.000 description 1
- 206010043554 thrombocytopenia Diseases 0.000 description 1
- 206010043778 thyroiditis Diseases 0.000 description 1
- 239000003106 tissue adhesive Substances 0.000 description 1
- 230000005944 tissue migration Effects 0.000 description 1
- 239000012929 tonicity agent Substances 0.000 description 1
- 231100000041 toxicology testing Toxicity 0.000 description 1
- 230000008733 trauma Effects 0.000 description 1
- 208000003982 trichinellosis Diseases 0.000 description 1
- 201000007588 trichinosis Diseases 0.000 description 1
- 201000008827 tuberculosis Diseases 0.000 description 1
- 229920001664 tyloxapol Polymers 0.000 description 1
- MDYZKJNTKZIUSK-UHFFFAOYSA-N tyloxapol Chemical compound O=C.C1CO1.CC(C)(C)CC(C)(C)C1=CC=C(O)C=C1 MDYZKJNTKZIUSK-UHFFFAOYSA-N 0.000 description 1
- 229960004224 tyloxapol Drugs 0.000 description 1
- 230000002792 vascular Effects 0.000 description 1
- 239000003981 vehicle Substances 0.000 description 1
- 230000001018 virulence Effects 0.000 description 1
- 230000009278 visceral effect Effects 0.000 description 1
- 208000029257 vision disease Diseases 0.000 description 1
- 230000004393 visual impairment Effects 0.000 description 1
- 230000002747 voluntary effect Effects 0.000 description 1
- 229940018272 xeomin Drugs 0.000 description 1
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K9/00—Medicinal preparations characterised by special physical form
- A61K9/0012—Galenical forms characterised by the site of application
- A61K9/0019—Injectable compositions; Intramuscular, intravenous, arterial, subcutaneous administration; Compositions to be administered through the skin in an invasive manner
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/56—Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/56—Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids
- A61K31/57—Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids substituted in position 17 beta by a chain of two carbon atoms, e.g. pregnane or progesterone
- A61K31/573—Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids substituted in position 17 beta by a chain of two carbon atoms, e.g. pregnane or progesterone substituted in position 21, e.g. cortisone, dexamethasone, prednisone or aldosterone
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/56—Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids
- A61K31/58—Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids containing heterocyclic rings, e.g. danazol, stanozolol, pancuronium or digitogenin
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/715—Polysaccharides, i.e. having more than five saccharide radicals attached to each other by glycosidic linkages; Derivatives thereof, e.g. ethers, esters
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/02—Inorganic compounds
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/30—Macromolecular organic or inorganic compounds, e.g. inorganic polyphosphates
- A61K47/34—Macromolecular compounds obtained otherwise than by reactions only involving carbon-to-carbon unsaturated bonds, e.g. polyesters, polyamino acids, polysiloxanes, polyphosphazines, copolymers of polyalkylene glycol or poloxamers
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/30—Macromolecular organic or inorganic compounds, e.g. inorganic polyphosphates
- A61K47/36—Polysaccharides; Derivatives thereof, e.g. gums, starch, alginate, dextrin, hyaluronic acid, chitosan, inulin, agar or pectin
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/30—Macromolecular organic or inorganic compounds, e.g. inorganic polyphosphates
- A61K47/36—Polysaccharides; Derivatives thereof, e.g. gums, starch, alginate, dextrin, hyaluronic acid, chitosan, inulin, agar or pectin
- A61K47/40—Cyclodextrins; Derivatives thereof
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K9/00—Medicinal preparations characterised by special physical form
- A61K9/0012—Galenical forms characterised by the site of application
- A61K9/0048—Eye, e.g. artificial tears
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P19/00—Drugs for skeletal disorders
- A61P19/02—Drugs for skeletal disorders for joint disorders, e.g. arthritis, arthrosis
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P29/00—Non-central analgesic, antipyretic or antiinflammatory agents, e.g. antirheumatic agents; Non-steroidal antiinflammatory drugs [NSAID]
Definitions
- the present invention relates to viscous formulations and to methods for treating and/or preventing various peripheral diseases and conditions by peripheral administration to a patient of a viscous formulation.
- Peripheral administration includes intradermal, subdermal, subcutaneous, intramuscular, intra-articular (i.e. to treat an articular pathology such as a knee or facet joint osteoarthritis) and epidural (i.e. to treat a radiculopathy, spondylitis, and spondylosis [also known as degenerative disc disease, spinal arthritis, osteoarthritis of the spine]) routes of administration.
- the administration can be carried out, for example, by injection, insertion or implantation of the viscous formulation.
- the present invention relates to extended release and sustained release viscous formulations, including injectable implants, for treating various non-ophthalmic inflammatory and/or painful conditions, such as skin or joint pain and/or inflammation, radicular pain from nerve root irritation or inflammation, or chronic back pain from spondylosis or spondylitis.
- a pharmaceutical composition is a formulation which contains at least one active ingredient (for example an anti-inflammatory polymer such as a polymeric hyaluronic acid and/or a corticosteroid such as a triamcinolone) as well as, for example, one or more excipients, buffers, carriers, stabilizers, preservatives and/or bulking agents, and is suitable for administration to a patient to achieve a desired effect or result.
- active ingredient for example an anti-inflammatory polymer such as a polymeric hyaluronic acid and/or a corticosteroid such as a triamcinolone
- excipients for example, buffers, carriers, stabilizers, preservatives and/or bulking agents
- the pharmaceutical compositions disclosed herein can have diagnostic, therapeutic, cosmetic and/or research utility in various species, such as for example in human patients or subjects.
- hyaluronic acid also called hyaluronan and sodium hyaluronate
- Hyaluronic acid is most frequently referred to as hyaluronan due to the fact that it exists in vivo as a polyanion and not in the protonated acid form.
- U.S. Pat. Nos. 4,636,524; 4,713,448; 5,099,013, and 5,143,724 disclose particular hyaluronans or hyaluronic acids and methods for making them.
- intra-articular use of a hyaluronic acid i.e.
- hyaluronic acid formulations include JuvedermTM (Allergan), an injectable dermal filler comprised of a cross-linked hyaluronic acid. Also known are Orthovisc® (Anika), Durolane (Smith & Nephew), Hyalgan® (Sanofi), Hylastan® (Genzyme), Supartz® (Seikagaku/Smith & Nephew)), Synvisc® (Genzyme), Euflexxa®, (Ferring) which are used as injectable (intra-articular) hyaluronic acid viscosupplements, of various molecular weights with various degrees of cross-linking of the hyaluronic acid, for treating osteoarthritis joint pain.
- compositions for therapeutic or cosmetic use comprising a high molecular weight hyaluronic acid and one or more active agents has been disclosed. See e.g. U.S. patent application Ser. Nos. 11/039,192; 11/695,527; 11/742,350; 10/966,764; 11/354,415, and; 11/741,366.
- corticosteroids can have anti-inflammatory properties.
- intra-articular corticosteroids have been used to treat various joint diseases. See e.g. Zulian F., et al., Triamcinolone acetonide and hexacetonide intra - articular treatment of symmetrical joints in juvenile idiopathic arthritis: a double - blind trial , Rheum 2004; 43:1288-1291. (use of 2 mg to 80 mg of triamcinolone acetonide) and; Hertzberger-ten Cate R.
- intramuscular steroids have been given to treat acute conditions, until the patient can be managed by use of oral steroids, such as asthma (Mancinelli L. et al., Intramuscular high - dose triamcinolone acetonide in the treatment of severe chronic asthma , West J Med November 1997:167(5); 322-329 [up to 360 mg of the triamcinolone was administered daily for three days to a patient]).
- Subcutaneous and intradermal administration of a steroid is not a preferred route of administration because dermal atrophy can result.
- the risk of dermal atrophy by the steroid can be reduced by giving the injection in a deep gluteal muscle area and avoiding leakage of the steroid formulation into the dermis.
- Such steroid particles can induce an inflammatory response upon administration. This may occur because macrophages present at the administration site can be unable to remove the steroid particles (by phagocytosis) which have a large morphology and irregular geometry. Indeed such particles can be toxic to macrophages and lead to cell death. The death of macrophages then leads to release of pro-inflammatory cytokines that cause both acute and chronic inflammation. Clinical examples of toxicity from particles include gouty arthritis, where urate crystals that range from 5 to 20 microns can cause arthritis. See eg.
- a triamcinolone pharmaceutical composition available under the trade name Kenalog® (Bristol-Myers-Squibb, Princeton N.J.) has been used to treat various conditions by intramuscular or intra-articular (intrabursal use) administration.
- Each milliliter (ml) of Kenalog® 40 composition comprises 40 milligrams (mg) of triamcinolone acetonide, sodium chloride as a tonicity agent, 10 mg (0.99%) benzyl alcohol as a preservative, 7.5 mg (0.75%) of carboxymethylcellulose sodium and 0.4 mg (0.04%) of polysorbate 80 as resuspension aids.
- Benzyl alcohol preservative and/or polysorbate 80 can potentially be toxic to sensitive tissues.
- preservative-containing corticosteroid formulations have been linked to cases of adhesive arachnoiditis following epidural injections exacerbating a patient's back pain. See e.g. Hurst, E. W., Adhesive Arachnoiditis and Vascular Blockage caused by Detergents and Other Chemical Irritants: an Experimental Study . J. Path. Bact., 1955. 70: p. 167; DeLand, F. H., Intrathecal toxicity studies with benzyl alcohol . Toxicol Appl Pharmacol, 1973. 25(2): p. 153, and; Hetherington, N. J. and M. J. Dooley, Potential for patient harm from intrathecal administration of preserved solutions . Med J Aust, 2000. 173(3): p. 141.
- the triamcinolone acetonide in Kenalog® rapidly separates and precipitates from the remainder of the formulation. For example, if Kenalog® is left standing for as short a time as about five to ten minutes a substantial separation of a triamcinolone acetonide precipitate from the remainder of the composition occurs.
- Such rapid settling of the triamcinolone also occurs with other known saline based suspensions of triamcinolone (with or with preservatives and stabilizers).
- a substantially uniform suspension (which is not provided by Kenalog or other saline based suspensions of triamcinolone) would be beneficial to provide a consistent and accurate dose upon administration of the suspension.
- resuspension processing requires the use of the resuspension aids noted above which can affect sensitive tissues.
- a corticosteroid such as triamcinolone
- administration of known formulations of a corticosteroid can also result in an allergic or inflammatory reaction possibly due to the burst or high release rates of triamcinolone from the known formulations.
- a reaction can also be due to or be exacerbated due to the large and irregular size of the insoluble corticosteroid particles administered.
- FIG. 1 is a flow chart which summarizes a preferred manufacturing process for making the triamcinolone formulations of Examples 1 to 9.
- FIG. 2 consists of three graphs showing the size (diameter) in microns (x-axis) of triamcinolone acetonide particles in three commercial lots of Kenalog-40 vs the frequency of occurrence of the measured particles diameters.
- Triamcinolone acetonide particle size diameter and distribution was determined by laser light scattering using a Horiba LA 300 instrument.
- FIG. 3 consists of four bar graphs (A, B, C and D) showing the size (diameter) in microns (x-axis) of the triamcinolone acetonide particles raw material used to make the Trivaris formulations disclosed herein formulation vs the frequency of occurrence of the measured particles diameters.
- the line graph in FIGS. 3A to 3D shows the area under the curve for cummulative (%) triamcinolone acetonide particle size (right hand side y axis). Triamcinolone acetonide particle size diameter and distribution was determined by laser light scattering using a Horiba LA 300 instrument.
- the present invention provides viscous formulations and methods for treating and/or preventing various peripheral conditions by peripheral administration to a patient of a viscous formulation.
- Peripheral administration includes intradermal, subdermal, subcutaneous, intramuscular, intra-articular (i.e. to treat an articular pathology such as knee or facet joint osteoarthritis), and epidural (i.e. to treat a radiculopathy, spondylitis, and spondylosis [a.k.a. degenerative disc disease, spinal arthritis, osteoarthritis of the spine]), routes of administration.
- the peripheral administration can be carried out, for example, by injection, insertion or implantation of the viscous formulation.
- the present invention relates to extended release and sustained release viscous formulations, including injectable implants, for treating various non-ophthalmic inflammatory and/or painful conditions, such as skin or joint pain and/or inflammation, radicular pain from nerve root irritation or inflammation, or chronic back pain from spondylosis or spondylitis.
- the present invention provides sterile, preservative-free, sustained release viscous formulations for treating peripheral conditions with the desirable characteristics of low immunogenicity, lack of toxic preservatives or surfactants in the formulation, and sustained release the active agent.
- administering means the step of giving (i.e. administering) a pharmaceutical composition to a subject.
- the pharmaceutical compositions disclosed herein can be “locally administered”, that is administered at or in the vicinity of the site at which a therapeutic result or outcome is desired. For example to treat an peripheral condition by peripheral administration of a viscous formulation.
- sustained release means release of an active agent (such as a corticosteroid and/or an anti-inflammatory hyaluronic acid) over a period of about seven days or more, while “extended release” means release of an active agent over a period of time of less than about seven days.
- Essentially free means that only trace amounts of the substance can be detected.
- Peripheral administration means the step of administering a viscous formulation by a route of administration which is not an intraocular administration and which is also not an immediate systemic administration (such as an intravenous administration or oral ingestion) of the viscous formulation.
- peripheral administration excludes intravenous and oral administrations but includes, for example, subdermal, intradermal, subcutaneous, intramuscular and intra-articular routes of administration.
- Peripheral condition means a non-ophthalmic disease or condition, such as a dermatologic, articular, allergic, inflammatory and/or painful disease or condition, such as an arthritic condition.
- peripheral conditions that can be treated by peripheral intramuscular or intra-articular administration include allergies, asthma, dermatitis, drug hypersensitivity reactions, rhinitis, serum sickness, transfusion reactions, dermatologic conditions, bullous dermatitis herpetiformis, exfoliative erythroderma, mycosis fungoides, pemphigus, severe erythema multiforme (Stevens-Johnson syndrome), endocrine disorders, drenocortical insufficiency, adrenal hyperplasia, hypercalcemia, thyroiditis, enteritis, colitis, anemia, aplasia, thrombocytopenia, trichinosis, meningitis, leukemia, lymphomas, multiple sclerosis, cerebral edema, craniotomy, head injury, proteinuria, n
- Peripheral location means a location on or within the periphery of a mammalian body.
- a peripheral locations includes locations on or within the skin, a voluntary (striated) muscle, such as on or within an arm or leg, within a joint (intra-articular) and all anatomical areas near and within the vertebral column.
- Intraocular and visceral that is within the gut, gut cavity, viscera, internal organs, GI, GU, etc system are not peripheral locations.
- “Pharmaceutical composition” means a formulation in which an active ingredient (the active agent) can be an anti-inflammatory polymer (such as a polymeric hyaluronic acid) and/or a steroid, such as a corticosteroid, such as a triamcinolone.
- the word “formulation” means that there is at least one additional ingredient in the pharmaceutical composition besides the active agent.
- a pharmaceutical composition is therefore a formulation which is suitable for diagnostic or therapeutic administration (i.e. by peripheral injection or by insertion of a depot or implant) to a subject, such as a human patient.
- substantially free means present at a level of less than one percent by weight of the pharmaceutical composition.
- sustained release means release of an active agent (such as a triamcinolone) over a period of about seven days or more, while “extended release” means release of an active agent over a period of time of less than about seven days.
- the present compositions are highly suitable for peripheral administration to a peripheral location.
- the present compositions are advantageously substantially free of added preservative components, for example, contain no benzyl alcohol preservative.
- the present compositions advantageously require no resuspension aid or aids.
- the present compositions are easily and effectively injectable into a peripheral location of a patient's body and can be maintained as a substantially uniform suspension for long periods of time, for example, at least about one week or more, without resuspension processing, for example, without requiring shaking or other agitating of the composition to obtain substantial suspension uniformity.
- the present compositions and methods provide substantial enhancements and advantages, for example, relative to the prior art Kenalog® 40 composition and methods of using such prior art composition.
- compositions useful for injection into a peripheral location can comprise a corticosteroid component, a viscosity inducing component, and an aqueous carrier component.
- the corticosteroid component is present in a therapeutically effective amount.
- the corticosteroid component can be present in the compositions in a plurality of particles.
- compositions can include a corticosteroid component in an amount of up to about 25% (w/v) or more of the composition.
- the corticosteroid component is present in an amount of at least about 80 mg/ml of composition.
- the corticosteroid component is present in an amount in a range of about 1% to about 10% or about 20% (w/v) of the composition.
- the corticosteroid component comprises triamcinolone acetonide.
- the viscosity inducing component is present in an amount effective in increasing the viscosity of the composition. Any suitable, preferably ophthalmically acceptable, viscosity inducing component may be employed in accordance with the present invention.
- the viscosity inducing component is present in an amount in a range of about 0.5% to about 20% (w/v) of the composition.
- the viscosity inducing component is a hyaluronic acid polymer component, such as sodium hyaluronate.
- the preferred Hyaluronic acid (“HA”) used in the formulations disclosed as the preferred viscosity inducing component has the following characteristics.
- the HA provides an increase in viscosity but has a high shear rate, meaning that it retains syringeability through 25-30 gauge needles.
- the HA is a natural component of the extracellular matrix of many mammalian tissues therefore providing a biocompatible viscosity inducing component.
- the HA is a tissue adhesive so that when HA is injected into a tissue such as a muscle diffusion and migration of the HA through fascial planes in minimized. See e.g. Cohen et al. Biophys J. 2003; 85: 1996-2005.
- a poorly adhesive polymer such as silicone can migrate through tissues.
- tissue adhesion and therefore low tissue migration characteristic of a formulation which comprises HA enables the formulation to remain largely at the injection site.
- a corticosteroid-HA formulation will have the advantageous characteristic of low diffusion out of the peripheral location, such as an intra-articular location (i.e. to treat facet joint arthritis).
- a botulinum toxin-HA formulation will have the advantageous characteristic of low diffusion out of the peripheral location, such as an intramuscular location (i.e. into the small orbicularis muscle to treat hemifacial spasm).
- use of HA in a formulation can limit drug or biologic exposure to surrounding or adjacent non-target tissues, thereby limiting side effects (with regard to para-ocular botulinum toxin administration) such as ptosis or visual impairment.
- a carrier or the active agent i.e. steroid crystals
- solubilized contact with water is required.
- the preferred HA used provides this through an ability to become hydrated (absorb water).
- the HA used is a polymer that can be cross-linked to varying degrees, thereby permitting alteration of characteristics such as rate of HA migration for the peripheral location of administration, rate of active agent diffusion and migration out of the HA carrier.
- the present compositions have a viscosity of at least about 10 cps or at least about 100 cps, preferably at least about 1,000 cps, more preferably at least about 10,000 cps and still more preferably at least about 70,000 cps, for example, up to about 250,000 cps, or about 300,000 cps, at a shear rate of 0.1/second.
- the present compositions are structured or have make-ups so as to be injectable into a peripheral location of a human or animal body preferably through a 27 gauge needle, more preferably through a 29 or 30 gauge needle.
- the corticosteroid component is present in a plurality of particles which are substantially uniformly suspended in the composition and remain substantially uniformly suspended in the composition for at least about 1 week, preferably at least about 2 weeks or at least about 1 month, and still more preferably at least about 6 months or at least about 1 year or at least about 2 years, without requiring resuspension processing, that is, without requiring being shaken or otherwise agitated to maintain the corticosteroid component particles substantially uniformly suspended in the composition.
- compositions having such substantially uniform suspension of corticosteroid component particles, so as to be able to provide a consistent and accurate dose upon administration provide substantial advantages relative to the prior art.
- the present compositions may be manufactured, shipped and stored for substantial periods of time without the corticosteroid component particles precipitating from the remainder of the composition. Having the corticosteroid component particles maintained substantially uniformly suspended in the composition allows the composition to provide long term dosing consistency and accuracy per unit dose amount administered, without any need to resuspend the corticosteroid particles.
- the aqueous carrier component is advantageously biocompatible and may include one or more conventional expedients.
- the carrier component may include an effective amount of at least one of a preservative component, a tonicity component and a buffer component.
- the present compositions include no added preservative component. This feature reduces or minimizes or even substantially eliminates adverse reactions upon administration which may be caused by or linked to the presence of a preservative component.
- a resuspension component may be employed in accordance with the present invention, in many instances, because of the ability of the present composition to remain a substantially uniform suspension for a long period of time without requiring resuspension processing, the compositions advantageously contain no added resuspension components.
- Such methods comprise administering, e.g. injecting a corticosteroid component-containing composition, for example, a composition in accordance with the present intention to a peripheral location.
- Such administering is effective in providing a desired therapeutic effect.
- the administering step advantageously comprises at least one of intramuscular or intra-articular injecting.
- the composition can comprise a triamcinolone present in a therapeutically effective amount as a plurality of particles; a viscosity inducing component in an amount effective to increase the viscosity of the composition, and; an aqueous carrier component.
- the composition can have a viscosity of at least about 10 cps at a shear rate of about 0.1/second and is injectable into a peripheral location, for example through a 27 gauge needle. By reducing the viscosity of our formulation it can be injected into the peripheral through a 28, 29 or 30 gauge needle.
- the triamcinolone particles of the pharmaceutical composition are substantially uniformly suspended in the composition and the viscosity inducing component is a polymeric hyaluronate.
- a detailed embodiment within the scope of our invention is a pharmaceutical composition for treating a peripheral condition, comprising triamcinolone particles; polymeric hyaluronate, in which the triamcinolone particles are suspended; sodium chloride; sodium phosphate, and water.
- the pharmaceutical composition can have a viscosity at a shear rate of about 0.1/second of between about 80,000 cps to about 300,000, preferably from about 100,000 cps to about 300,000 cps, and most preferably from about 1280,000 cps to about 225,000 cps.
- the pharmaceutical composition can have a viscosity at a shear rate of about 0.1/second of between about 80,000 cps and about 300,000 cps, and that when the pharmaceutical composition has a viscosity at a shear rate of about 0.1/second of between about 100,000 cps and about 150,000 cps it can be injected into a peripheral location through a 27, 28, 29 or 30 gauge needle.
- the sodium phosphate present in the pharmaceutical composition can comprise both monobasic sodium phosphate and dibasic sodium phosphate.
- the pharmaceutical composition can comprise between about 2% w/v triamcinolone and about 8% w/v triamcinolone, between about 2% w/v hyaluronate and about 3% w/v hyaluronate, about 0.6% w/v sodium chloride and about 0.03% w/v sodium phosphate to about 0.04% w/v sodium phosphate.
- the pharmaceutical composition of claim 5 can comprise between about 0.5% w/v hyaluronate and about 6% w/v hyaluronate. If desired the hyaluronate can be heated (see Example 11) to decrease its molecular weight (and therefore its viscosity) in the formulation.
- the pharmaceutical composition can also comprises between about 0.6% w/v sodium chloride to about 0.9% w/v sodium chloride. Generally, more sodium chloride is used in the formulation as less phosphate is used in the formulation, for example 0.9% sodium chloride can be used if no phosphate is present in the formulation, as in this manner the tonicity of the formulation can be adjusted to obtain the desired isotonicity with physiological fluid.
- the pharmaceutical composition can comprise between about 0.0% w/v sodium phosphate and 0.1% w/v sodium phosphate. As noted, more phosphate can be used in the formulation if less sodium chloride is present in the formulation so as to obtain a desired pH 7.4 buffering effect.
- a more detailed embodiment within the scope of our invention is a pharmaceutical composition for treating a peripheral condition, the pharmaceutical composition consisting essentially of triamcinolone particles, polymeric hyaluronate, in which polymeric hyaluronate the triamcinolone particles are suspended, sodium chloride, sodium phosphate, and water.
- the pharmaceutical composition can have a viscosity at a shear rate 0.1/second at 25° C. of between about 128,000 cps and about 225,000 cps and the sodium phosphate present in the pharmaceutical composition can be present as both monobasic sodium phosphate and dibasic sodium phosphate.
- the most preferable viscosity range is 140,000 to 280,000 cps at a shear rate 0.1/second at 25° C.
- a further embodiment of our invention is a triamcinolone suspension for treating a peripheral condition, consisting of triamcinolone particles, polymeric hyaluronate, in which the triamcinolone particles are suspended, sodium chloride, dibasic sodium phosphate heptahydrate, monobasic sodium phosphate monohydrate, and water, wherein the composition has a viscosity at a shear rate 0.1/second of between about 128,000 cps and about 225,000 cps.
- Our invention also includes a method for treating a peripheral condition by administering (as by injecting) the pharmaceutical composition set forth above to the peripheral of a human or animal, thereby treating the peripheral condition.
- a method for treating a peripheral condition edema by administering to a peripheral location pharmaceutical composition comprising a triamcinolone, and a hyaluronate, wherein the pharmaceutical composition having a viscosity at a shear rate 0.1/second of between about 128,000 cps and about 225,000 cps.
- a pharmaceutical composition within the scope of our invention for treating a peripheral condition can comprise a triamcinolone present in a therapeutically effective amount as a plurality of particles, a viscosity inducing component in an amount effective to increase the viscosity of the composition, and an aqueous carrier component, wherein the composition has a viscosity of at least about 10 cps at a shear rate of 0.1/second and is injectable into a peripheral location and wherein the pharmaceutical composition releases the triamcinolone with substantially first order release kinetics over a period of at least about 45 days after the peripheral injection or administration.
- This pharmaceutical composition can exhibit reduced generation of inflammation, no plume effect (that is no wide dispersion of the triamcinolone into the peripheral as soon as the triamcinolone is injected), and cohesiveness (as shown by the retention of the form of the triamcinolone gel for 30 weeks or longer after peripheral injection of the triamcinolone gel formulation) upon peripheral injection of the pharmaceutical composition.
- Our invention encompasses a method for treating a peripheral condition, the method comprising the step of peripheral administration of a sustained release pharmaceutical composition implant comprising a triamcinolone present in a therapeutically effective amount as a plurality of particles, a viscosity inducing component in an amount effective to increase the viscosity of the composition, and an aqueous carrier component, wherein the composition has a viscosity of at least about 10 cps at a shear rate of 0.1/second and is injectable into a peripheral location, and wherein the peripheral condition is treated for up to about 30 weeks by the triamcinolone released from the viscous formulation.
- a sustained release pharmaceutical composition implant comprising a triamcinolone present in a therapeutically effective amount as a plurality of particles, a viscosity inducing component in an amount effective to increase the viscosity of the composition, and an aqueous carrier component, wherein the composition has a viscosity of at least about 10 cps at a shear
- the pharmaceutical composition can comprise triamcinolone particles, polymeric hyaluronate, in which the triamcinolone particles are suspended, sodium chloride, sodium phosphate, and water.
- the peripheral administration can be injected through a 27 gauge needle into the peripheral location, and in an aggregate number of patients practise of the method results in less peripheral inflammation than does practise of the same method with a second pharmaceutical composition which is a saline solution or suspension of a triamcinolone.
- Our invention also includes a process for making a pharmaceutical composition by (a) mixing triamcinolone particles about 4 microns to about 8 microns in diameter with sodium chloride crystals, and about 35% to about 40% of the total volume of the water (water for injection) used to make the formulation; (b) heating the triamcinolone and sodium chloride mixture to a temperature between about 120° C.
- a pharmaceutical composition for treating a peripheral condition comprising a plurality of corticosteroid particles mixed with a viscous polymer, wherein the pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C., and the pharmaceutical composition can be injected into a peripheral location through a 25 to 33 gauge needle.
- the corticosteroid particles can have a substantially uniform diameter, as shown for example by FIGS. 3A , 3 B, 3 C and 3 D. Additionally, preferably substantially all (i.e. up to 90-97%) of the corticosteroid particles are embedded within the viscous polymer.
- the corticosteroid can be a triamcinolone and the viscous polymer can be a polymeric hyaluronate or a polymeric hyaluronic acid.
- An alternate method for treating a peripheral condition can comprise the step of injecting into a peripheral location of a patient with a peripheral condition a viscous pharmaceutical composition comprising a plurality of corticosteroid particles mixed into a viscous polymeric matrix, wherein the pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C., such that about one hour after the peripheral injection only about 10% or less (or only about 5% or less or only about 3% or less) of the corticosteroid particles are present in the peripheral free of the polymeric matrix.
- An alternate process for making an pharmaceutical composition for peripheral administration can comprise the step of mixing an aqueous suspension of a plurality of corticosteroid particles and an aqueous solution of a viscous polymeric matrix, so that the resulting pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C.
- the corticosteroid particles can have a median particle size of between about 4 microns and about 5 microns.
- the corticosteroid particles can have a stable diameter for at least three months after the pharmaceutical has been made and stored for three months in a syringe placed horizontally at about 25° C. at about 60% relative humidity.
- Our invention also includes a pharmaceutical composition for treating an articular pathology, the pharmaceutical composition comprising a plurality of corticosteroid particles mixed with a viscous polymer, wherein the pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C.
- Our invention also includes a method for treating an articular pathology, the method comprising the step of injecting into a joint of a patient with an articular pathology (such as a joint or spine inflammation) a viscous pharmaceutical composition comprising a plurality of corticosteroid particles mixed into a viscous polymeric matrix, wherein the pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C.
- an articular pathology such as a joint or spine inflammation
- Our invention includes a method for treating a peripheral condition, the method comprising the step of administering to a peripheral location of a human body a viscous formulation comprising a viscous polymer, wherein the viscous formulation has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C., thereby treating at least one symptom of the peripheral condition.
- the peripheral condition can be an articular pathology.
- the peripheral location can be an intra-articular location.
- the step of administering can be carried out by injecting.
- the viscous formulation can comprises a plurality of corticosteroid particles mixed with the viscous polymer.
- the corticosteroid can be a triamcinolone.
- the viscous polymer can be a polymeric hyaluronate or a polymeric hyaluronic acid.
- Our invention also include a method for treating a peripheral condition, the method comprising the step of injecting into a peripheral location of a patient with a peripheral condition a viscous formulation comprising a plurality of corticosteroid particles mixed into a viscous polymeric matrix, wherein the pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C., such that about one hour after the peripheral injection only about 10% or less of the corticosteroid particles are present at the peripheral location free of the polymeric matrix. About one hour after the peripheral injection only about 3-5% or less of the corticosteroid particles can be present at the peripheral location free of the polymeric matrix.
- Our invention also includes a method for treating arthritis, the method comprising the step of injecting into a joint of a patient with arthritis a viscous formulation comprising a plurality of corticosteroid particles mixed into a viscous polymeric matrix, wherein the viscous formulation has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C.
- Our invention also includes a method for treating a peripheral condition, the method comprising the steps of (a) administering to a peripheral location of a human body a viscous formulation comprising a viscous polymer, wherein the viscous formulation has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C., thereby treating at least one symptom of the peripheral condition, and; (b) administering to a peripheral location of a human body a plurality of corticosteroid particles, thereby treating at least one symptom of the peripheral condition.
- the plurality of corticosteroid particles can be mixed with the viscous polymer.
- our invention includes a method for treating a peripheral condition of a patient selected from the group of peripheral conditions consisting of osteoarthritis, radiculopathy, spondylitis, and spondylosis, the method comprising the step of injecting into a peripheral location of the a viscous formulation comprising a plurality of corticosteroid particles mixed into a viscous polymeric matrix, wherein the pharmaceutical composition has a viscosity of between about 130,000 cps and about 300,000 cps at a shear rate of about 0.1/second at about 25° C.
- the present invention is based upon our discovery of viscous formulations specifically designed for peripheral injection to treat various peripheral conditions.
- Our viscous formulations have numerous superior characteristics and advantages, including the following when the viscous formulation is a viscous steroid formulation: (1) the steroid present in our formulations does not rapidly settle out from or precipitate from the formulations.
- our formulations have a shelf life of at least two years, meaning that our formulations can be left standing for up to about two years before peripheral administration, and after two years the formulation can still provide a consistent and accurate dose of the steroid upon peripheral injection to the formulation; (2) our formulations are free of preservatives and resuspension aids, such as benzyl alcohol and/or a polysorbate; (3) concomitantly, our formulations have a much reduced inflammatory and toxicity effect; (4) as well as being sterile and preservative-free our viscous steroid formulations can provide sustained release of therapeutic amounts of the steroid over multi-month periods upon peripheral injection of such formulations.
- our viscous suspension steroid formulations are sustained release implants; (5) peripheral administration of our viscous formulations is not associated with an increased incidence of adverse events such as inflammation; (6) our viscous formulations permit steroid particles (crystals) to be released (as they solubilize) from a discrete unitary location, thereby avoiding a plume effect (rapid dispersion) characteristic of aqueous steroid formulations upon administration, and; (7) the sustained release characteristic of our formulations reduces the need for peripheral administration of large drug quantities to achieve a desired therapeutic effect.
- the present invention provides viscous formulations useful for peripheral administration to a human or animal to treat a peripheral condition.
- An important aspect of our invention is the finding that upon a peripheral administration a rapid dispersion of the steroid particles can be reduced by formulating the steroid with a polymer that increases the formulation viscosity and that causes the steroid particles to agglomeration after the peripheral administration. This advantageously decreases steroid particle exposure to the tissues and reduces the inflammatory response. Post-injection inflammation is also reduced by eliminating form the formulation preservatives, such as benzyl alcohol, that have been shown to cause local tissue toxicity and inflammation.
- the triamcinolone used is preferably a triamcinolone acetonide because of the superior therapeutic properties of triamcinolone acetonide as compared to other forms of triamcinolone.
- post-injection joint inflammation associated with intra-articular application of a corticosteroid formulation can be decreased by: (1) reducing the particle size of the corticosteroid to ⁇ 10 microns with the morphology of the particle preferably being uniform or substantially; (2) adding a polymer to increase the viscosity of the corticosteroid formulation to reduce steroid particle dispersion within the joint, and (3) limiting the use of preservatives in the formulation.
- a preferred formulation for treating an articular (joints) condition can be a viscous formulation comprises of particles of a steroid (such as triamcinolone acetonide) which have a median particle size of ⁇ 10 microns and a substantially uniform shape.
- the steroid particles are mixed with a hyaluronic acid, a preferred polymer due to its anti-inflammatory properties.
- hyaluronic acid a polysaccharide double helix which can inhibit lymphocytes.
- Hyaluronic acid is naturally found in high concentrations in the synovial fluid and serves as a joint lubricant, shock absorber, and it reduces friction between the articular surfaces.
- hyaluronic acid supplementation into the joint synovium has a chondroprotective affect through multiple mechanisms and has been found to be disease-modifying as well as a symptom-modifying in patients with osteoarthritis.
- Our invention includes a viscous formulation which can be used as a single dose application and which is preservative-free and which does not cause post-injection aseptic endophthalmitis, a condition analogous to crystal-induced synovitis.
- Our viscous formulations have an optimal steroid particle size, a hyaluronic acid component, and no preservatives and can be use to treat peripheral conditions such as rheumatoid arthritis and osteoarthritis, and spinal conditions such as facet arthritis, and patients requiring epidural or spinal root injections for chronic pain.
- Hyaluronic acid has been injected into facial tissue to smooth out wrinkles and folds, especially around the nose, mouth (nasolabial folds), and forehead (glabellar folds).
- Hyaluronic acid has also used for increasing dermal volume to improve the appearance of scars that may be related to trauma or acne. Reduced lip and earlobe volume occurring with age can be improved with injections of hyaluronic acid. Chin and cheek augmentation can be effectively accomplished with local injections of hyaluronic acid.
- facial soft-tissue volume replacement using hyaluronic acid including that produced from non-animal sources, have been associated with post-injection inflammatory responses. (Pinheiro M.
- a steroid such as triamcinolone
- Our invention includes a combination of low concentrations of a steroid with a hyaluronic acid to reduce post-injection inflammation.
- viscous formulations are not administered in a manner which provides an immediate systemic administration they can be does in a manner which permits a slow or controlled entry of the active agent into the systemic system of the patient.
- a slow or controlled entry of the active agent into the systemic system of the patient generally from 2.5 mg to 100 mg per day of the active agent steroid can be administered within the viscous formulation, depending on the disease or condition being treated.
- an initial dose can be of about 40 to 80 mg of a steroid in the viscous formulation injected deeply into a gluteal muscle (thereby preventing atrophy of subcutaneous fat).
- the equivalent milligram dosage of various glucocorticoids is cortisone 25, triamcinolone 4, hydrocortisone 20, paramethasone 2, prednisolone 5, betamethasone 0.75, prednisone 5, dexamethasone 0.75 and methylprednisolone 4.
- compositions within the scope of our invention can comprise a corticosteroid component; a viscosity inducing component; and an aqueous carrier component.
- the compositions are advantageously biocompatible.
- the present viscous formulations are advantageously substantially free of added preservative components.
- the present viscous formulations preferably include no added resuspension component, such as polysorbate-80, which is included in the Kenalog®-40 composition.
- the viscous formulations can include a corticosteroid component.
- a corticosteroid component is present in the compositions in a therapeutically effective amount, that is in an amount effective in providing a desired therapeutic effect.
- the corticosteroid component is present in the composition in a plurality of particles. Any suitable corticosteroid component may be employed in according to the present invention.
- Such corticosteroid component advantageously has a limited solubility in water, for example, at 25° C.
- the corticosteroid component preferably has a solubility in water at 25° C. of less than 10 mg/ml.
- One particularly useful characteristic of the presently useful corticosteroid components is the ability of such component to reduce inflammation.
- corticosteroid components examples include, without limitation, cortisone, prednesolone, triamcinolone, triamcinolone acetonide, fluorometholone, dexamethosone, medrysone, loteprednol, derivatives thereof and mixtures thereof.
- the term “derivative” refers to any substance which is sufficiently structurally similar to the material of which it is identified as a derivative so as to have substantially similar functionality or activity, for example, therapeutic effectiveness, as the material when the substance is used in place of the material.
- the corticosteroid component comprises triamcinolone acetonide.
- the corticosteroid component advantageously is present in an amount of at least about 10 mg per ml of the composition.
- One important advantage of the present invention is the effective ability of the present compositions to include relatively large amounts or concentrations of the corticosteroid component.
- the corticosteroid component may be present in the present compositions in an amount in the range of about 1% or less to about 5% or about 10% or about 20% or about 30% or more (w/v) of the composition.
- the present compositions include more than about 4% (w/v), for example at least about 5% (w/v), to about 10% (w/v) or about 20% (w/v) or about 30% (w/v) of the corticosteroid component.
- about 50 ⁇ L of our Example 8 or 9 formulation provide respectively 2 mg and 4 mg of triamcinolone. This is in contrast to other formulations (such as Kenalog 40) which require 100 ⁇ L to provide 4 mg of triamcinolone.
- the viscosity inducing component is present in an effective amount in increasing, advantageously substantially increasing, the viscosity of the composition.
- increasing the viscosity of the compositions to values well in excess of the viscosity of water, for example, at least about 100 cps at a shear rate of 0.1/second at 25 degrees C, compositions which are highly effective.
- the relatively high viscosity of the present compositions are believed to enhance the ability of the present compositions to maintain the corticosteroid component particles in substantially uniform suspension in the compositions for prolonged periods of time, for example, for as long as 1 to 2 years, without requiring resuspension processing.
- the relatively high viscosity of the present compositions may also have an additional benefit of at least assisting the compositions to have the ability to have an increased amount or concentration of the corticosteroid component, as discussed elsewhere herein, for example, while maintaining such corticosteroid component in substantially uniform suspension for prolonged periods of time.
- the present compositions have viscosities of at least about 10 cps or at least about 100 cps or at least about 1000 cps, more preferably at least about 10,000 cps and still more preferably at least about 70,000 cps or more, for example up to about 200,000 cps or about 250,000 cps, or about 300,000 cps or more, at a shear rate of 0.1/second.
- the present compositions not only have the relatively high viscosity as noted above but also have the ability or are structured or made up so as to be effectively placeable, e.g., injectable preferably through a 27 gauge needle, or even through a 30 gauge needle.
- the presently useful viscosity inducing components preferably are shear thinning components in that as the present composition containing such a shear thinning viscosity inducing component is injected through a narrow space, such as 27 gauge needle, under high shear conditions the viscosity of the composition is substantially reduced during such passage. After such passage, the composition regains substantially its pre-injection viscosity so as to maintain the corticosteroid component particles in suspension.
- any suitable viscosity inducing component for example, biocompatible viscosity inducing component, may be employed in accordance with the present invention.
- the viscosity inducing component is present in an amount effective in providing the desired viscosity to the composition.
- the viscosity inducing component is present in an amount in a range of about 0.5% or about 1.0% to about 5% or about 10% or about 20% (w/v) of the composition.
- the specific amount of the viscosity inducing component employed depends upon a number of factors including, for example and without limitation, the specific viscosity inducing component being employed, the molecular weight of the viscosity inducing component being employed, the viscosity desired for the present composition being produced and/or used and the like factors, such as shear thinning.
- the viscosity inducing component is chosen to provide at least one advantage, and preferably multiple advantages, to the present compositions, for example, in terms of each of injectability into a peripheral location viscosity, sustainability of the corticosteroid component particles in suspension, for example, in substantially uniform suspension, for a prolonged period of time without resuspension processing, bio compatibility with tissues into which the composition is to be placed and the like advantages.
- the viscosity inducing component preferably comprises a polymeric component and/or at least one viscoelastic agent.
- useful viscosity inducing components include, but are not limited to, hyaluronic acid (such as a polymeric hyaluronic acid), carbomers, polyacrylic acid, cellulosic derivatives, polycarbophil, polyvinylpyrrolidone, gelatin, dextrin, polysaccharides, polyacrylamide, polyvinyl alcohol, polyvinyl acetate, derivatives thereof and mixtures and copolymers thereof.
- hyaluronic acid such as a polymeric hyaluronic acid
- carbomers polyacrylic acid, cellulosic derivatives, polycarbophil, polyvinylpyrrolidone, gelatin, dextrin, polysaccharides, polyacrylamide, polyvinyl alcohol, polyvinyl acetate, derivatives thereof and mixtures and copolymers thereof.
- the molecular weight of the presently useful viscosity inducing components may be in a range of about 10,000 Daltons or less to about 2 million Daltons or more. In one particularly useful embodiment, the molecular weight of the viscosity inducing component is in a range of about 100,000 Daltons or about 200,000 Daltons to about 1 million Daltons or about 1.5 million Daltons. Again, the molecular weight of the viscosity inducing component useful in accordance with the present invention, may vary over a substantial range based on the type of viscosity inducing component employed, and the desired final viscosity of the present composition in question, as well as, possibly one or more other factors.
- a viscosity inducing component is a polymeric hyaluronate component, for example, a metal hyaluronate component, preferably selected from alkali metal hyaluronates, alkaline earth metal hyaluronates and mixtures thereof, and still more preferably selected from sodium hyaluronates, and mixtures thereof.
- the molecular weight of such hyaluronate component i.e. a polymeric hyaluronic acid
- the present compositions include a polymeric hyaluronate component in an amount in a range about 0.05% to about 0.5% (w/v).
- the hyaluronate component is present in an amount in a range of about 1% to about 4% (w/v) of the composition.
- the very high polymer viscosity forms a gel that slows particle sedimentation rate to the extent that often no resuspension processing is necessary over the estimated shelf life, for example, at least about 2 years, of the composition.
- Such a composition may be marketed in pre-filled syringes since the gel cannot be easily removed by a needle and syringe from a bulk container. Pre-filled syringes have the advantages of convenience for the injector and the safety which results from less handling.
- the aqueous carrier component is advantageously ophthalmically acceptable and may include one or more conventional excipients useful in ophthalmic compositions.
- the present compositions preferably include a major amount of liquid water.
- the present compositions may be, and are preferably, sterile, for example, prior to being administered.
- the present compositions preferably include at least one buffer component in an amount effective to control the pH of the composition and/or at least one tonicity component in an amount effective to control the tonicity or osmolality of the compositions. More preferably, the present compositions include both a buffer component and a tonicity component.
- the buffer component and tonicity component may be chosen from those which are conventional and well known in the art.
- buffer components include, but are not limited to, acetate buffers, citrate buffers, phosphate buffers, borate buffers and the like and mixtures thereof. Phosphate buffers are particularly useful.
- Useful tonicity components include, but are not limited to, salts, particularly sodium chloride, potassium chloride, mannitol and other sugar alcohols, and other suitable ophthalmically acceptably tonicity component and mixtures thereof.
- the amount of buffer component employed preferably is sufficient to maintain the pH of the composition in a range of about 6 to about 8, more preferably about 7 to about 7.5.
- the amount of tonicity component employed preferably is sufficient to provide an osmolality to the present compositions in a range of about 200 to about 400, more preferably about 250 to about 350, mOsmol/kg respectively.
- the present compositions are substantially isotonic.
- the present compositions may include one or more other components in amounts effective to provide one or more useful properties and/or benefits to the present compositions.
- the present compositions may be substantially free of added preservative components, in other embodiments, the present compositions include effective amounts of preservative components, preferably such components which are more compatible with or friendly to tissues into which the composition is placed than benzyl alcohol.
- preservative components include, without limitation, benzalkonium chloride, chlorhexidine, PHMB (polyhexamethylene biguanide), methyl and ethyl parabens, hexetidine, chlorite components, such as stabilized chlorine dioxide, metal chlorites and the like, other ophthalmically acceptable preservatives and the like and mixtures thereof.
- the concentration of the preservative component, if any, in the present compositions is a concentration effective to preserve the composition, and is often in a range of about 0.00001% to about 0.05% or about 0.1% (w/v) of the composition.
- the present composition may include an effective amount of resuspension component effective to facilitate the suspension or resuspension of the corticosteroid component particles in the present compositions.
- the present compositions are free of added resuspension components.
- effective amounts of resuspension components are employed, for example, to provide an added degree of insurance that the corticosteroid component particles remain in suspension, as desired and/or can be relatively easily resuspended in the present compositions, such resuspension be desired.
- the resuspension component employed in accordance with the present invention if any, is chosen to be more compatible with or friendly to the tissues into which the composition is placed than polysorbate 80.
- resuspension component Any suitable resuspension component may be employed in accordance with the present invention.
- resuspension components include, without limitation, surfactants such as poloxanes, for example, sold under the trademark Pluronic®; tyloxapol; sarcosinates; polyethoxylated castor oils, other surfactants and the like and mixtures thereof.
- vitamin derivatives include, without limitation, Vitamin E tocopheryl polyethylene glycol succinates, such as Vitamin E tocopheryl polyethylene glycol 1000 succinate (Vitamin E TPGS).
- useful vitamin derivatives include, again without limitation, Vitamin E tocopheryl polyethylene glycol succinamides, such as Vitamin E tocopheryl polyethylene glycol 1000 succinamide (Vitamin E TPGSA) wherein the ester bond between polyethylene glycol and succinic acid is replaced by an amide group.
- the presently useful resuspension components are present, if at all, in the compositions in accordance with the present invention in an amount effective to facilitate suspending the particles in the present compositions, for example, during manufacture of the compositions or thereafter.
- the specific amount of resuspension component employed may vary over a wide range depending, for example, on the specific resuspension component being employed, the specific composition in which the resuspension component is being employed and the like factors. Suitable concentrations of the resuspension component, if any, in the present compositions are often in a range of about 0.01% to about 5%, for example, about 0.02% or about 0.05% to about 1.0% (w/v) of the composition.
- the availability of minimally soluble corticosteroid components, such as triamcinolone acetonide, to peripheral tissues may be limited by the dissolution rate for these substances. Slow dissolution is both good and bad for the patient.
- the mean elimination half-life for triamcinolone acetonide is advantageously quite long, for example, about 19 days in nonvitrectonized patients and measurable drug levels are detected for up to about 3 months.
- therapeutic drug levels in the peripheral location may not be achieved for about 1 to about 3 days, due to the slow dissolution rate of the corticosteroid component particles.
- an effective amount of a solubilizing component is provided in the composition to solubilize a minor amount, that is less than 50%, for example in a range of 1% or about 5% to about 10% or about 20% of the corticosteroid component.
- a cyclodextrin component such as ⁇ -cyclodextrin, sulfo-butylether ⁇ -cyclodextrin (SBE), other cyclodextrins and the like and mixtures thereof, at about 0.5 to about 5.0% (w/v) solubilizes about 1 to about 10% of the initial dose of triamcinolone acetonide. This presolubilized fraction provides a readily bioavailable loading dose, thereby avoiding any delay time in therapeutic effectiveness.
- solubilizing component is advantageous to provide any relatively quick release of the corticosteroid component into the peripheral location for therapeutic effectiveness.
- solubilizing component should be biocompatible acceptable or at least sufficiently compatible with the tissues into which the composition is placed to avoid undue damage to the tissue.
- the pharmacokinetics of the corticosteroid component for example, triamcinolone acetonide
- peripheral administration may involve both the rate of drug dissolution and the rate of drug efflux via the anterior route.
- triamcinolone acetonide concentration peaks (monitored in aqueous humor) after several days at thousands of nanograms per mL. This peak (C max ) is followed by a rapid decrease lasting about 200 hours, and ends in a slow elimination phase with a half-life of about 19 days.
- Patients typically require repeat dosing, for example about every three months.
- compositions further contain sustained release components, for example, polymers (in the form for example of gels and microspheres), such as poly (D,L,-lactide) or poly(D,L-lactide co-glycolide), in amounts effective to reduce local diffusion rates and/or corticosteroid particle dissolution rates.
- sustained release components for example, polymers (in the form for example of gels and microspheres), such as poly (D,L,-lactide) or poly(D,L-lactide co-glycolide), in amounts effective to reduce local diffusion rates and/or corticosteroid particle dissolution rates.
- the sustained release component is preferably biodegradable or bioabsorbable so that no residue remains over the long term.
- the amount of the delayed release component included may very over a relatively wide range depending, for example, on the specific sustained release component is being employed, the specific release profile desired and the like factors. Typical amounts of delayed release components, if any, included in the present compositions are in a range of about 0.05 to 0.1 to about 0.5 or about 1 or more percent (w/v) (weight of the ingredient in the total volume of the composition) of the composition.
- the present compositions can be prepared using suitable blending/processing techniques or techniques, for example, one or more conventional blending techniques.
- the preparation processing should be chosen to provide the present compositions in forms which are useful for placement or injection into a peripheral location of humans or animals.
- a concentration corticosteroid component dispersion is made by combining the corticosteroid component with water, and the excipient (other than the viscosity inducing component) to be included in the final composition.
- the ingredients are mixed to disperse the corticosteroid component and then autoclaved.
- the steroid powder may be ⁇ -irradiated before addition to the sterile carrier.
- the viscosity inducing component may be purchased sterile or sterilized by conventional processing, for example, by filtering a dilute solution followed by lyophylization to yield a sterile powder.
- the sterile viscosity inducing component is combined with water to make an aqueous concentrate.
- the concentrated corticosteroid component dispersion can be blended or mixed and added or combined as a slurry to the viscosity inducing component concentrate. Water is added in a quantity sufficient (q.s.) to provide the desired composition and the composition is mixed until homogenous.
- Methods of using the present composition are provided and are included within the scope of the present invention.
- such methods comprise administering a composition in accordance with the present invention to a peripheral location of a human or animal, thereby obtaining a desired therapeutic effect.
- the present methods may comprise a single injection into a peripheral location or may involve repeated injections, for example over periods of time ranging from about one week or about 1 month or about 3 months to about 6 months or about 1 year or longer.
- compositions are as follows:
- Example 2 Triamcinolone acetonide 2% (w/v) 2% (w/v) 4% (w/v) 4% (w/v) Sodium Hyaluronate 0.05% (w/v) 0.5% (w/v) 0.05% (w/v) 0.5% (w/v) (0.6 ⁇ 10 6 DALTONS) Sodium Phosphate 0.4% (w/v) 0.4% (w/v) 0.4% (w/v) 0.4% (w/v) 0.4% (w/v) Vitamin E-TPGS 0.5% (w/v) 0.5% (w/v) 0.0 0.0 ⁇ -cyclodextrin 0.5% (w/v) 0.5% (w/v) 0.0 0.0 Water for Injection q.s. q.s. q.s. Viscosity at shear rate 20 cps 500 cps 20 cps 500 cps 0.1/second at 25° C.
- compositions are prepared as follows.
- a concentrated triamcinolone acetonide dispersion is made by combining triamcinolone acetonide with water, Vitamin E-TPGS and ⁇ -cyclodextrin, if any. These ingredients are mixed to disperse the triamcinolone acetonide, and then autoclaved.
- the sodium hyaluronate may be purchased as a sterile powder or sterilized by filtering a dilute solution followed by lyophylization to yield a sterile powder.
- the sterile sodium hyaluronate is dissolved in water to make an aqueous concentrate.
- the concentrated triamcinolone acetonide dispersion is mixed and added as a slurry to the sodium hyaluronate concentrate. Water is added q.s. (quantum sufficit, as much as suffices, in this case as much as is required to prepare the homogenous mixture, dispersion, gel or suspension) and the mixture is mixed until homogenous.
- compositions produced a loose flocculation of triamcinolone acetonide that is easily re-suspended by gentle inversion.
- compositions can be marketed in small volume pharmaceutical grade glass bottles, and are found to be therapeutically effective against various peripheral conditions when peripherally administered.
- compositions are as follows:
- Example 6 Triamcinolone acetonide 2.0% (w/v) 4.0% (w/v) 8.0% (w/v) Sodium hyaluronate 3.0% (w/v) 2.5% (w/v) 2.0% (w/v) Sodium Phosphate 0.4% (w/v) 0.4% (w/v) 0.4% (w/v) Water for Injection q.s. q.s. q.s. Viscosity at shear rate 0.1/ 300,000 cps 180,000 cps 100,000 cps second at 25° C.
- compositions are prepared in a manner substantially analogous to that set forth in Example 1.
- compositions substantially slows the particle sedimentation rate to an extent that no resuspension processing is necessary or required over the estimated shelf life, e.g., about 2 years, of the compositions.
- These compositions can be marketed in prefilled syringes since they can not easily be removed by a needle and syringe from a container. However, with the compositions in prefilled syringes, the compositions can be effectively injected intramuscular or intra-articular using a 27 gauge or a 30 gauge needle to provide a desired therapeutic effect.
- compositions of Examples 5 to 7 employ or contain a sufficient concentration of high molecular weight sodium hyaluronate so as to form a gelatinous plug or drug depot upon peripheral administration to a peripheral location.
- Triamcinolone acetonide particles are, in effect, trapped or held within this viscous plug, so that undesirable pluming does not occur, and the risk of drug particles disadvantageously settling directly on the tissue is substantially reduced, for example, relative to using a composition with a water-like viscosity, such as Kenalog® 40. Since sodium hyaluronate solutions are subject to dramatic shear thinning, these formulations are easily injected through 27 gauge or even 30 gauge needles.
- compositions are as follows:
- Example 9 Triamcinolone acetonide 2.0% (w/v) 8.0% (w/v) Sodium hyaluronate 2.5% (w/v) 2.3% (w/v) (polymeric) Sodium chloride 0.63% (w/v) 0.63% (w/v) dibasic sodium phosphate, 0.30% (w/v) 0.30% (w/v) heptahydrate Monobasic sodium phosphate, 0.04% (w/v) 0.04% (w/v) monohydrate Water for Injection q.s. q.s. Viscosity at shear rate 170,000 ⁇ 25% cps 200,000 ⁇ 25% cps 0.1/second at 25° C.
- compositions are prepared in a manner substantially analogous to that set forth in Example 1.
- compositions substantially slows the particle sedimentation rate to an extent that no resuspension processing is necessary or required over the estimated shelf life, e.g., about 2 years, of the compositions.
- These compositions can be marketed in prefilled syringes since they can not easily be removed by a needle and syringed from a container. However, with the compositions in prefilled syringes, the compositions can be effectively injected into a peripheral location using a 27 gauge or a 30 gauge needle to provide a desired therapeutic effect.
- the sodium hyaluronate powders used in these compositions have water contents in a range of about 4% to about 20%, preferably about 4% to about 8%, by weight. Differences in the average molecular weight of the hyaluronate used can result in variation in the viscosity of compositions in accordance with the present invention which have the same nominal chemical make-ups.
- the viscosities indicated herein should be understood to be target viscosities, with the composition being acceptable for use if the actual viscosity of the composition is within plus or minus ( ⁇ ) about 25% or about 30% or about 35% of the target viscosity.
- each of the compositions set forth in the Examples has a density of about 1 gm/ml
- the percentages set forth herein as being based on weight per volume (w/v) can also be considered as being based on weight per weight (w/w).
- compositions of Examples 8 and 9 employ or contain a sufficient concentration of high molecular weight (i.e. polymeric) sodium hyaluronate so as to form a gelatinous plug or drug depot upon peripheral injection into s peripheral location.
- high molecular weight (i.e. polymeric) sodium hyaluronate i.e. polymeric
- the average molecular weight of the hyaluronate used is less than about 2 million, and more preferably the average molecular weight of the hyaluronate used is between about 1.3 million and 1.6 million.
- the triamcinolone acetonide particles are, in effect, trapped or held within this viscous plug of hyaluronate, so that undesirable pluming does not occur upon peripheral injection of the formulation.
- the most preferred viscosity range for the Example 8 and 9 formulations is 140,000 cps to 280,000 cps at a shear rate 0.1/second at 25° C.
- the triamcinolone acetonide used in the formulations set forth herein has the is chemical name 9-Fluoro-11,21-dihydroxy-16,17-[1-methylethylidenebis(oxy)]pregna-1,4-diene-3,20-dione, and can have the following structure
- Triamcinolone acetonide has a very low solubility in water of only about 0.11 mg/ml to about 0.13 mg/mL.
- Loftsson T. et al. Determination of Aqueous Solubility by Heating and Equilibration: A Technical Note, AAPS PharmSciTech. 2006; 7(1): Article 4.DOI: 10.1208/pt070104, and; Yang J. et al., Transdermal delivery system of triamcinolone acetonide from a gel using phonophoresis , Arch Pharm Res 29(5); 412-417: 2006.
- the Examples 8 and 9 formulations are prepared as sterile products of a uniform, opaque white dispersion of microfine triamcinolone acetonide particles suspended in a hyaluronate-based polymeric hydrogel, intended for peripheral injection.
- the Examples 8 and 9 formulations can be used to treat, for example, arthritis (i.e. rheumatoid and osteoarthritis) and various allergic and dermatologic conditions.
- the Examples 8 and 9 formulations are formulated using only excipients that are fully biocompatible (i.e. non-toxic).
- the Examples 8 and 9 formulations (2% (w/w) and 8% (w/w) triamcinolone acetonide, respectively) are buffered at physiological pH with a low concentration of sodium phosphate salts; rendered isotonic with sodium chloride, and use Water for Injection, USP, as the vehicle.
- a target dosage of 1 mg of the triamcinolone acetonide active agent can be delivered in a 50 mg (approximately 48 ⁇ L) injection of the Example 8 2% (w/w) triamcinolone acetonide gel suspension formulation.
- a target dosage of 4 mg of the triamcinolone acetonide active agent can be delivered in a 50 mg (approximately 48 ⁇ L) injection of the Example 9 8% (w/w) triamcinolone acetonide gel suspension formulations.
- the triamcinolone present in our formulations does not rapidly, or even slowly, settle out from or precipitate from the formulations.
- our Example 8 and 9 formulations have a shelf life of at least two years, meaning that these formulations can be left standing (without agitation) for up to about two years before peripheral administration, and after two years the same formulations can still provide a consistent and accurate dose of triamcinolone upon injection to the formulation.
- the composition of triamcinolone 2% injectable gel suspension is triamcinolone 2.0% (w/w), sodium hyaluronate, sodium chloride, dibasic sodium phosphate (heptahydrate), monobasic sodium phosphate (monohydrate), and water for injection).
- the composition of triamcinolone 8% injectable gel suspension is triamcinolone 8.0% (w/w), sodium hyaluronate, sodium chloride, dibasic sodium phosphate (heptahydrate), monobasic sodium phosphate (monohydrate), and water for injection.
- the triamcinolone acetonide injectable gel suspension we have invented is a viscous suspension of triamcinolone acetonide formulated at concentrations of 8% and 2% with sodium hyaluronate, sodium chloride, dibasic sodium phosphate (heptahydrate), monobasic sodium phosphate (monohydrate), and water for injection (i.e. the formulations of Examples 8 and 9 respectively).
- the suspensions are prepared to have physiologic pH, and to be isotonic, and preservative-free.
- the Examples 8 and 9 suspensions can be supplied in single-use glass syringes with fixed 27 gauge needles.
- the syringes are overfilled to 0.17-0.18 mL, and calibrated to deliver 0.05 mL when primed to a black or blue mark on the barrel of the syringe to thereby provide the 2% and 8% suspensions to deliver 1 mg and 4 mg of triamcinolone, respectively (the pre-filled syringes are made by Allergan, Inc., Irvine, Calif.). These syringes have a shelf life of at least about two years when stored at 2-8° C.
- a preferred formulation such as that of Examples 8 and 9 can be used to treat a peripheral condition by intramuscular injection, but formulated to contain up to 160 mg of the triamcinolone in the formulation injected.
- the injection is carried out by intramuscular injection into the gluteal muscles of either or both legs to treat eg an acute exacerbation of multiple sclerosis symptoms.
- Hay fever can be treated by injecting the gluteal muscle with the Example 8 or Example 9 formulation formulated to contain 40 to 80 mg (i.e. 60 mg) of the triamcinolone.
- Example 8 or Example 9 formulation formulated to contain 2.5 to 5 mg triamcinolone (for a smaller joint and from 5 to 40 mg triamcinolone for a larger joint.
- Intramuscular or intra-articular administration of the Example 8 or Example 9 formulation can be use to treat pain (as in arthritis, such as osteoarthritis) administering (a) a cross-linked (with more cross-linking the hyaluronic acid will reside in the joint for a longer period) or not cross-linked hyaluronic acid, followed by (b) administration of a steroid (i.e. 1-8 wt % triamcinolone (for a greater effect to decrease inflammation) followed by (c) administration of just a hyaluronic acid by itself.
- a steroid i.e. 1-8 wt % triamcinolone
- An alternate method can be intramuscular or intra-articular administration of the Example 8 or Example 9 formulation followed by use of a hyaluronic acid by itself (for the lubrication and anti-inflammation effect of the hyaluronic acid).
- Our invention comprises triamcinolone acetonide injectable gel suspensions formulated viscous suspensions of triamcinolone acetonide at concentrations of, for example, 8% and 2% with sodium hyaluronate, sodium chloride, dibasic sodium phosphate (heptahydrate), monobasic sodium phosphate (monohydrate), and water for injection.
- the triamcinolone acetonide injectable gel suspensions are preferably at physiologic pH, isotonic, and preservative-free.
- Triamcinolone acetonide injectable gel suspensions within the scope of our invention can be supplied in single-use glass syringes with fixed 27 gauge needles.
- the syringes can be overfilled to 0.17-0.18 mL, and calibrated to deliver 0.05 mL when primed to a black mark on the barrel of the syringe to thereby deliver, for example, 2% and 8% suspensions of 1 mg and 4 mg of triamcinolone, respectively.
- Our triamcinolone acetonide injectable gel suspensions can be defined as implants which upon injection (i.e. implantation) into a peripheral location provided sustained release (i.e. over a period of up to seven months or longer) from the compact gel bolus injected.
- the triamcinolone particles are not available to and/or are substantially ignored by macrophages due to the aggregation (suspension) of the triamcinolone particles in the high molecular weight hyaluronate used in our formulations.
- the fact that our triamcinolone formulations are in situ forming implants can also limit the exposure of whole or individual triamcinolone crystals to sensitive peripheral tissues, concomitantly thereby limiting macrophage activation and hence also limiting or preventing an peripheral inflammatory response.
- our formulation maintains the triamcinolone crystals in a collective matrix that acts as a sustained-release reservoir which decrease the need for frequent repeat injections.
- our formulation forms a cohesive agglomerate upon peripheral injection.
- the reduced surface area of such an agglomerate facilitates provision and maintenance of a lower release rate of the triamcinolone, as compared to much larger surface area saline suspension of a triamcinolone (such as Kenalog).
- the cohesiveness of our formulation is exemplified by the fact that the formulation maintains its internal consistency (i.e. its shape after injection) for at least about 30 weeks after injection.
- compositions of our invention are preferably formulated with hyaluronic acid, a material known for its anti-inflammatory abilities.
- Hyaluronic acid a novel, double helical molecule , Science, 1973 Feb. 9; 179(73):560-2.
- preservatives and/or stabilizers such as benzyl alcohol and polysorbate 80
- our formulation reduces the retinal toxicity of our formulations as compared to formulations which contain one or more preservatives and/or stabilizers.
- a preferred embodiment of our invention can be the Example 8 and 9 formulations in which the average diameter of the triamcinolone particles present in the formulations is less than 10 microns and preferably less than 5 microns, and additionally with a uniform (spherical) morphology. It has been shown in the pulmonary literature that micronized particles of corticosteroids, ⁇ 10 microns, and preferably ⁇ 5 microns, are less injurious to macrophages, and have the potential for less inflammation. Thus, preparing our formulations with a median triamcinolone particle size of ⁇ 5 microns and with uniform shape provides formulation which are even more biocompatible in the peripheral and with less propensity to cause peripheral location inflammation.
- the triamcinolone formulations are made as sterile, uniform, opaque white gel suspensions suitable for peripheral injection.
- the manufacturing process involves two main stages: 1) sterile suspension bulk compounding and 2) aseptic filling.
- the bulk product manufacture includes preparations of three separate parts, followed by aseptic combination of these three parts.
- the aseptic filling operation is conducted in a class 100 environment, and the sterile bulk product may be filled into pre-sterilized ready-to-use syringes.
- Part I is prepared in a main batch vessel that has capabilities of bulk heat sterilization and viscous fluid mixing.
- WFI water for injection
- Triamcinolone powder is then added and dispersed with strong agitation.
- the suspension is heated and sterilized at above 121° C. for a sufficient time period by steam passing through the jacket of the vessel. After the bulk heat cycle is completed, the suspension is cooled down to room temperature.
- Part II is prepared in an open vessel equipped with a top entering, variable speed mixer. First, WFI at 10% of batch size is charged into the vessel. Sodium phosphate salts and, optionally, a ⁇ -cyclodextrin derivative is added and dissolved. If necessary, the pH of the solution is adjusted with 1 N sodium hydroxide and/or 1 N hydrochloric acid. When a beta cyclodextrin is used in the formulation is can be dissolved along with the phosphate salts in this part II.
- Part III is prepared in a Class 100 environment through a series of aseptic procedures. First, sodium hyaluronate is dissolved in WFI at dilute concentration, e.g., 0.2% w/w. The solution is sterile-filtered and sodium hyaluronate powder is recovered through bulk lyophilization. Finally, the sodium hyaluronate powder is reconstituted with sterile WFI at 50% of batch size.
- Sterile bulk suspension is compounded by aseptically combining (mixing) the three parts.
- Part II solution is filtered into sterile Part I in the main batch vessel using a 0.2 micron sterilizing grade filter.
- Part III is then aseptically transferred into the main batch vessel.
- the bulk is blended (mixed) under low shear conditions to achieve uniformity.
- the final bulk suspension is held in a controlled area before aseptic filling.
- Aseptic filling operations are performed in a Class 100 environment. Sterile bulk suspension is first filtered through a clarification screen into a sterile holding container. The bulk is then transferred to the filling machine and filled into pre-sterilized syringes. The filled units are transferred to the packaging area for application of tamper-evident seals, labeling and cartoning.
- Example 15 for making triamcinolone sterile suspensions is illustrated by the FIG. 1 process flow chart.
- Part III can be heated at between about 120° C. and about 130° C. for between about 25-35 minutes. Doing so both sterilizes the hyaluronate and can reduce the initial 1 million to 1.9 million Daltons molecular weight of the hyaluronate used in our formulation by about 20% to about 30% (i.e. to between about 0.7 million to about 1.3 million Daltons), thereby permitting use of a higher (i.e. 30 gauge) gauge injection needle.
- Example 9 a viscous formulation comprising 2-8 wt % triamcinolone acetonide in polymeric hyaluronic acid, referred to herein by the trade name Trivaris.
- Trivaris 2% The findings set forth herein apply as well to the Example 8 formulation (Trivaris 2%).
- Trivaris 2% We confirmed the low immunogenicity or anti-inflammatory nature of Trivaris and determined that upon administration substantially all the Trivaris triamcinolone acetonide particles are embedded within the polymeric matrix of the hyaluronic acid and that Trivaris is storage stable.
- a major factor associated with the inflammatory reaction characteristic of sterile endophthalmitis can be the drug particle burden at the site of peripheral administration, as evidenced by the plume effect, which can occur upon peripheral injection of an aqueous (low viscosity) TA formulation.
- individual drug particles are recognized by resident macrophages as they attempt to phagocytose free floating drug particles. Phagocytosis leads to cytokine release and both neutrophils and macrophages are thereby recruited.
- indigestible drug particles released by an aqueous TA formulation can be lethal to macrophages and neutrophils, causing these cells die and release lysosomal contents, oxidative enzymes, and more proinflammatory cytokines. This results in an acceleration of the inflammatory reaction and hence the clinical manifestations of sterile endophthalmitis.
- Kenalog-40 Three lots of Kenalog-40 were examined (see FIG. 2 ) and it was determined that the TA particles in Kenalog can be as large as 80 microns, with high particles size variability.
- This toxic inflammatory reaction to corticosteroid crystals has also been observed following intra-articular injections where an inflammatory joint reaction occurs within 48 hours after injection is called crystal synovitis.
- Other more remote causes of sterile endophthalmitis with use of peripheral corticosteroid formulations include the presence of endotoxins, extraneous particles and/or excipients in the formulation and the formulation having a pH less than 5 or greater than pH 8.
- the particles size distribution of four lots of triamcinolone acetonide particles (raw material) used to make the various Trivaris formulations was also examined. As shown by FIGS. 3A to 3D , the median TA particles size was between about 4 microns and 5 microns and 90% of the TA particles had a diameter of 10 microns or less. FIG. 3 also shows that about 40% of the TA particles had a diameter between about 4 microns and about 8 microns and that about 60% of the TA particles had a diameter between about 3.5 microns and about 9 microns.
- the TA particle size distribution data in FIGS. 2 and 3 was obtained by light scattering using a Horiba LA 300 instrument.
- the line graph in FIGS. 3A , B, C and 3 D shows the cummulative TA particle size % (area under the curve) (right hand side Y axis).
- Trivaris is a viscous TA formulation in which the TA drug particles are embedded in and coated by the polymeric matrix of the hyaluronic acid (HA) to thereby form a viscoelastic hydrogel with a viscosity of between about 130 k and about 300 k centipoises (cps) at a shear rate of about 0.1/second at 25° C.
- cps centipoises
- the TA drug particle sizes in Trivaris are deliberately uniform in distribution with a median particle size ranging from about 4 to about 6 microns.
- This hydrogel formulation of Trivaris can be injected through a hypodermic (syringe) needle having a needle gauge as small as 33 gauge.
- the HA in Trivaris creates a physical barrier to free movement of the embedded TA drug particles, thereby reducing the potential for free floating TA particle exposure in the peripheral and resulting macrophage activation.
- HA is recognized by scavenging peripheral macrophages as a native (non-immunogenic) because there is a high concentration of HA naturally present in the peripheral humor.
- coating the TA drug particles with HA renders the injected Trivaris formulation non-antigenic, lowering the potential of the TA drug particles to instigate an inflammatory response.
- HA encapsulation as an ‘immunologic disguise’ is used in a similar fashion by some streptococcus bacterial species to evade detection and phagocytosis by macrophages and increasing the virulence of the organism.
- the hydrogel formulation of Trivaris permits the TA particles to become free drug as the TA is solubilized (dissolves), thereby permitting the solubilized TA to enter solution and then diffuse or be actively transported to the retina to treat a retinal disease or condition.
- the close proximity of the TA drug particles in the Trivaris HA hydrogel allows for controlled and rapid agglomeration of the TA particles as the HA gradually diffuses over time out of the depot formed upon peripheral Trivaris injection.
- Trivaris The low numbers of drug particles in an unbound state following injection of Trivaris can be expected to reduce activation of scavenging macrophages compared with other TA suspensions, such as Kenalog-40, where the majority of the TA particles are upon peripheral injection exposed to macrophages and inflammatory consequences can then ensue.
- the effectiveness of the Trivaris formulation to reduce the inflammatory potential can be expected to reduce activation of scavenging macrophages compared with other TA suspensions, such as Kenalog-40, where the majority of the TA particles are upon peripheral injection exposed to macrophages and inflammatory consequences can then ensue.
- the effectiveness of the Trivaris formulation to reduce the inflammatory potential The effectiveness of the Trivaris formulation to reduce the inflammatory potential.
- Trivaris In addition to limiting particle exposure, the HA of Trivaris has additional inherent anti-inflammatory properties. Hyaluronic acid inhibits movement of macrophages, down regulates the production of proinflammatory cytokines and chemokines in models and human diseases, scavenges oxygen free radicals, and inhibits matrix metalloproteinases. Trivaris can include additional features to minimize an inflammatory reaction upon peripheral injection, such as preparing Trivaris to have a pH between 6 and 7 range, and strict endotoxin and extraneous particle control.
- the uniform population of micronized TA particles used to make Trivaris provides a predictable peripheral TA release pharmacokinetics with increased TA peripheral half-life.
- Trivaris formulations can also be used as an injectable pharmaceutical composition to treat various articular (joints and spine) pathologies while at the same time reducing the potential for occurrence of post-injection inflammation (crystal synovitis).
- the Trivaris formulation creates a physical barrier to free movement of drug particles to reduce the potential for particle exposure, macrophage activation, and the potential for sterile endophthalmitis.
- the consolidation of the TA drug particles in the HA hydrogel enables immediate recovery of vision after injection & enables PDT, thermal laser and diagnostic procedures to be performed.
- Incorporating a uniform population of micronized TA particles in the formulation facilitates management by macrophages when outside of the drug depot, but also leads to predictable peripheral pharmacokinetics with an increased peripheral half-life.
- Trivaris is supplied in pre-loaded syringes with little or no endotoxin and extraneous particle content, to thereby further limit post-injection inflammation.
- Trivaris is formulated to not contain benzyl alcohol or any other preservatives thereby reducing toxicity to peripheral location tissues upon peripheral administration of the formulation.
- An experiment can be carried out to evaluate the rate of release of a drug (i.e. cyclosporine, rapamycin or steroid such as triamcinolone acetonide) or a biologic (such as a botulinum toxin) from a high viscosity, high molecular weight carrier such as a polymeric hyaluronic acid. It can be determined that the rate of drug release of the drug or biologic is a function of extent of cross-linking of monomers of the polymeric carrier.
- a drug i.e. cyclosporine, rapamycin or steroid such as triamcinolone acetonide
- a biologic such as a botulinum toxin
- a botulinum toxin (such as BOTOX, DYSPORT, XEOMIN or MYOBLOC) can be formulated with a cross-linked hyaluronic acid to and administered as a dermal filler and wrinkle remover, thereby providing a prolonged residency of the botulinum toxin at the site of dermal administration and concomitantly a prolonged anti-wrinkle effect by the botulinum toxin.
- U.S. patent application publication number 2005 244358 discloses a method for reducing dermal lines by subdermal administration of a viscous chondroitin sulfate, hyaluronic acid and botulinum toxin type A composition.
- corticosteroid formulations set forth herein can be used to treat conditions including articular pathologies, such as rheumatoid and osteoarthritis, and spinal conditions, such as facet arthritis, and the treatment of chronic pain by epidural or spinal root injections of a formulation such as a Trivaris formulation
- the polymeric hyaluronate in Trivaris is a non-cross linked hyaluronate (so as to obtain, upon application of force to the plunger of the syringe used to administer Trivaris, a high shear rate and hence relative ease of injection of Trivaris through a 27-33 gauge needle)
- the hyaluronate can alternately be a cross linked hyaluronate (to form a true hydrogel therefore) with a significantly lower viscosity (i.e. with a viscosity of about 5,000 cps at a shear rate of about 0.1/second at about 25° C.).
- Such a cross-linked hyaluronate can have the same or similar excellent corticosteroid suspension property of Trivaris, and have the additional advantage of longer residency (i.e. biodegradable at a slower rate) of the hyaluronate in the peripheral, with resulting prolonged nominal immunogenicity of such a cross-linked hyaluronate formulation in the peripheral, due to a longer period of peripheral (or peripheral) retention of the corticosteroid particles in the polymeric matrix of the cross-linked hyaluronate.
- Cross-linked and non-cross linked hyaluronans can also be blended in various proportions to optimize syringeability while slowing biodegradation and improving long-term retention within inflammed tissues, such as in the treatment of osteoarthritis.
- cross-linked hyaluronate other cross-linked polymers can be used, such as for example a polycarbophil.
Landscapes
- Health & Medical Sciences (AREA)
- Chemical & Material Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Medicinal Chemistry (AREA)
- Pharmacology & Pharmacy (AREA)
- Animal Behavior & Ethology (AREA)
- General Health & Medical Sciences (AREA)
- Public Health (AREA)
- Veterinary Medicine (AREA)
- Epidemiology (AREA)
- Inorganic Chemistry (AREA)
- Dermatology (AREA)
- Ophthalmology & Optometry (AREA)
- Proteomics, Peptides & Aminoacids (AREA)
- Molecular Biology (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Organic Chemistry (AREA)
- General Chemical & Material Sciences (AREA)
- Chemical Kinetics & Catalysis (AREA)
- Rheumatology (AREA)
- Immunology (AREA)
- Orthopedic Medicine & Surgery (AREA)
- Engineering & Computer Science (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Physical Education & Sports Medicine (AREA)
- Pain & Pain Management (AREA)
- Pharmaceuticals Containing Other Organic And Inorganic Compounds (AREA)
- Medicinal Preparation (AREA)
Abstract
Description
| TABLE 1 | ||||
| Ingredient | Example 1 | Example 2 | Example 3 | Example 4 |
| Triamcinolone acetonide | 2% (w/v) | 2% (w/v) | 4% (w/v) | 4% (w/v) |
| Sodium Hyaluronate | 0.05% (w/v) | 0.5% (w/v) | 0.05% (w/v) | 0.5% (w/v) |
| (0.6 × 106 DALTONS) | ||||
| Sodium Phosphate | 0.4% (w/v) | 0.4% (w/v) | 0.4% (w/v) | 0.4% (w/v) |
| Vitamin E-TPGS | 0.5% (w/v) | 0.5% (w/v) | 0.0 | 0.0 |
| γ-cyclodextrin | 0.5% (w/v) | 0.5% (w/v) | 0.0 | 0.0 |
| Water for Injection | q.s. | q.s. | q.s. | q.s. |
| Viscosity at |
20 cps | 500 |
20 cps | 500 cps |
| 0.1/second at 25° C. | ||||
| TABLE 2 | |||
| Ingredient | Example 5 | Example 6 | Example 7 |
| Triamcinolone acetonide | 2.0% (w/v) | 4.0% (w/v) | 8.0% (w/v) |
| Sodium hyaluronate | 3.0% (w/v) | 2.5% (w/v) | 2.0% (w/v) |
| Sodium Phosphate | 0.4% (w/v) | 0.4% (w/v) | 0.4% (w/v) |
| Water for Injection | q.s. | q.s. | q.s. |
| Viscosity at shear rate 0.1/ | 300,000 cps | 180,000 cps | 100,000 cps |
| second at 25° C. | |||
| TABLE 3 | ||
| Ingredient | Example 8 | Example 9 |
| Triamcinolone acetonide | 2.0% (w/v) | 8.0% (w/v) |
| Sodium hyaluronate | 2.5% (w/v) | 2.3% (w/v) |
| (polymeric) | ||
| Sodium chloride | 0.63% (w/v) | 0.63% (w/v) |
| dibasic sodium phosphate, | 0.30% (w/v) | 0.30% (w/v) |
| heptahydrate | ||
| Monobasic sodium phosphate, | 0.04% (w/v) | 0.04% (w/v) |
| monohydrate | ||
| Water for Injection | q.s. | q.s. |
| Viscosity at shear rate | 170,000 ± 25% cps | 200,000 ± 25% cps |
| 0.1/second at 25° C. | ||
Claims (8)
Priority Applications (1)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US14/463,337 US9089478B2 (en) | 2003-11-12 | 2014-08-19 | Peripherally administered viscous formulations |
Applications Claiming Priority (7)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US51923703P | 2003-11-12 | 2003-11-12 | |
| US53006203P | 2003-12-16 | 2003-12-16 | |
| US10/966,764 US20050101582A1 (en) | 2003-11-12 | 2004-10-14 | Compositions and methods for treating a posterior segment of an eye |
| US11/354,415 US20060141049A1 (en) | 2003-11-12 | 2006-02-14 | Triamcinolone compositions for intravitreal administration to treat ocular conditions |
| US11/741,366 US20070224278A1 (en) | 2003-11-12 | 2007-04-27 | Low immunogenicity corticosteroid compositions |
| US11/828,561 US8846094B2 (en) | 2003-11-12 | 2007-07-26 | Peripherally administered viscous formulations |
| US14/463,337 US9089478B2 (en) | 2003-11-12 | 2014-08-19 | Peripherally administered viscous formulations |
Related Parent Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/828,561 Division US8846094B2 (en) | 2003-11-12 | 2007-07-26 | Peripherally administered viscous formulations |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| US20140356438A1 US20140356438A1 (en) | 2014-12-04 |
| US9089478B2 true US9089478B2 (en) | 2015-07-28 |
Family
ID=39101654
Family Applications (3)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/741,366 Abandoned US20070224278A1 (en) | 2003-11-12 | 2007-04-27 | Low immunogenicity corticosteroid compositions |
| US11/828,561 Active 2028-01-22 US8846094B2 (en) | 2003-11-12 | 2007-07-26 | Peripherally administered viscous formulations |
| US14/463,337 Expired - Lifetime US9089478B2 (en) | 2003-11-12 | 2014-08-19 | Peripherally administered viscous formulations |
Family Applications Before (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/741,366 Abandoned US20070224278A1 (en) | 2003-11-12 | 2007-04-27 | Low immunogenicity corticosteroid compositions |
| US11/828,561 Active 2028-01-22 US8846094B2 (en) | 2003-11-12 | 2007-07-26 | Peripherally administered viscous formulations |
Country Status (1)
| Country | Link |
|---|---|
| US (3) | US20070224278A1 (en) |
Cited By (3)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20160038396A1 (en) * | 2007-12-12 | 2016-02-11 | Allergan, Inc. | Dermal filler |
| US9833460B2 (en) | 2013-01-23 | 2017-12-05 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US10117938B2 (en) | 2015-01-21 | 2018-11-06 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
Families Citing this family (74)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| FR2861734B1 (en) | 2003-04-10 | 2006-04-14 | Corneal Ind | CROSSLINKING OF LOW AND HIGH MOLECULAR MASS POLYSACCHARIDES; PREPARATION OF INJECTABLE SINGLE PHASE HYDROGELS; POLYSACCHARIDES AND HYDROGELS OBTAINED |
| US20090148527A1 (en) * | 2007-12-07 | 2009-06-11 | Robinson Michael R | Intraocular formulation |
| US20060073208A1 (en) * | 2004-10-01 | 2006-04-06 | Allergan, Inc. | Cosmetic neurotoxin compositions and methods |
| US20070202186A1 (en) | 2006-02-22 | 2007-08-30 | Iscience Interventional Corporation | Apparatus and formulations for suprachoroidal drug delivery |
| US8197435B2 (en) * | 2006-05-02 | 2012-06-12 | Emory University | Methods and devices for drug delivery to ocular tissue using microneedle |
| AU2008256819A1 (en) | 2007-05-23 | 2008-12-04 | Allergan, Inc. | Cross-linked collagen and uses thereof |
| US8318695B2 (en) * | 2007-07-30 | 2012-11-27 | Allergan, Inc. | Tunably crosslinked polysaccharide compositions |
| US8697044B2 (en) | 2007-10-09 | 2014-04-15 | Allergan, Inc. | Crossed-linked hyaluronic acid and collagen and uses thereof |
| MX2010005331A (en) | 2007-11-16 | 2010-08-11 | Vicept Therapeutics Inc | Compositions and methods for treating purpura. |
| US20090143348A1 (en) * | 2007-11-30 | 2009-06-04 | Ahmet Tezel | Polysaccharide gel compositions and methods for sustained delivery of drugs |
| US8394784B2 (en) | 2007-11-30 | 2013-03-12 | Allergan, Inc. | Polysaccharide gel formulation having multi-stage bioactive agent delivery |
| US8394782B2 (en) | 2007-11-30 | 2013-03-12 | Allergan, Inc. | Polysaccharide gel formulation having increased longevity |
| US9044477B2 (en) * | 2007-12-12 | 2015-06-02 | Allergan, Inc. | Botulinum toxin formulation |
| US20120251615A1 (en) * | 2008-01-18 | 2012-10-04 | Horst Kief | Agent for intra-articular injection |
| US20090202645A1 (en) * | 2008-02-08 | 2009-08-13 | Acme Drugs S.R.L. | Intrasynovial formulations of stanozolol |
| KR101555293B1 (en) | 2008-03-11 | 2015-10-06 | 알콘 리서치, 리미티드 | Low viscosity, highly flocculated triamcinolone acetonide suspensions for intravitreal injection |
| US8399018B2 (en) * | 2008-07-21 | 2013-03-19 | Otonomy, Inc. | Controlled release ion channel modulator compositions and methods for the treatment of otic disorders |
| US8357795B2 (en) * | 2008-08-04 | 2013-01-22 | Allergan, Inc. | Hyaluronic acid-based gels including lidocaine |
| WO2010028025A1 (en) | 2008-09-02 | 2010-03-11 | Gurtner Geoffrey C | Threads of hyaluronic acid and/or derivatives thereof, methods of making thereof and uses thereof |
| US20100098772A1 (en) * | 2008-10-21 | 2010-04-22 | Allergan, Inc. | Drug delivery systems and methods for treating neovascularization |
| US20100104654A1 (en) | 2008-10-27 | 2010-04-29 | Allergan, Inc. | Prostaglandin and prostamide drug delivery systems and intraocular therapeutic uses thereof |
| US20100278897A1 (en) * | 2009-05-01 | 2010-11-04 | Allergan, Inc. | Intraocular bioactive agent delivery system with molecular partitioning system |
| US20100291027A1 (en) * | 2009-05-14 | 2010-11-18 | Jason Campbell | Hyaluronic acid (ha) injection vehicle |
| US8273725B2 (en) | 2009-09-10 | 2012-09-25 | Genzyme Corporation | Stable hyaluronan/steroid formulation |
| US20120245505A1 (en) | 2009-12-16 | 2012-09-27 | Robinson Michael R | Intracameral devices for sustained delivery |
| US9114188B2 (en) | 2010-01-13 | 2015-08-25 | Allergan, Industrie, S.A.S. | Stable hydrogel compositions including additives |
| US20110172180A1 (en) | 2010-01-13 | 2011-07-14 | Allergan Industrie. Sas | Heat stable hyaluronic acid compositions for dermatological use |
| US20110171286A1 (en) * | 2010-01-13 | 2011-07-14 | Allergan, Inc. | Hyaluronic acid compositions for dermatological use |
| US20110171311A1 (en) * | 2010-01-13 | 2011-07-14 | Allergan Industrie, Sas | Stable hydrogel compositions including additives |
| EP3085358B1 (en) | 2010-01-22 | 2017-11-01 | Allergan, Inc. | Intracameral sustained release therapeutic agent implants |
| AU2010348090B2 (en) | 2010-03-12 | 2015-09-03 | Allergan Industrie Sas | A fluid composition comprising a hyaluronan polymer and mannitol for improving skin condition |
| EP2550027B2 (en) | 2010-03-22 | 2019-03-20 | Allergan, Inc. | Polysaccharide and protein-polysaccharide cross-linked hydrogels for soft tissue augmentation |
| US9504643B2 (en) * | 2010-03-29 | 2016-11-29 | Evonik Corporation | Compositions and methods for improved retention of a pharmaceutical composition at a local administration site |
| US8883139B2 (en) | 2010-08-19 | 2014-11-11 | Allergan Inc. | Compositions and soft tissue replacement methods |
| US8889123B2 (en) | 2010-08-19 | 2014-11-18 | Allergan, Inc. | Compositions and soft tissue replacement methods |
| US9005605B2 (en) | 2010-08-19 | 2015-04-14 | Allergan, Inc. | Compositions and soft tissue replacement methods |
| US8697057B2 (en) | 2010-08-19 | 2014-04-15 | Allergan, Inc. | Compositions and soft tissue replacement methods |
| CN104758118B (en) | 2010-10-15 | 2018-04-06 | 科尼尔赛德生物医学公司 | For entering the device of eyes |
| US20120142628A1 (en) * | 2010-12-07 | 2012-06-07 | Allergan, Inc. | Methods for treating crepitus |
| EP2606828B1 (en) * | 2011-12-20 | 2018-04-11 | Angioclinic AG | Hyaluronic acid and its use for treating venous insufficiency and varicose veins |
| US20130096081A1 (en) | 2011-06-03 | 2013-04-18 | Allergan, Inc. | Dermal filler compositions |
| US9393263B2 (en) | 2011-06-03 | 2016-07-19 | Allergan, Inc. | Dermal filler compositions including antioxidants |
| CA3038735C (en) | 2011-06-03 | 2021-11-23 | Allergan, Inc. | Dermal filler compositions including antioxidants |
| US9408797B2 (en) | 2011-06-03 | 2016-08-09 | Allergan, Inc. | Dermal filler compositions for fine line treatment |
| US9662422B2 (en) | 2011-09-06 | 2017-05-30 | Allergan, Inc. | Crosslinked hyaluronic acid-collagen gels for improving tissue graft viability and soft tissue augmentation |
| US20130244943A1 (en) | 2011-09-06 | 2013-09-19 | Allergan, Inc. | Hyaluronic acid-collagen matrices for dermal filling and volumizing applications |
| TWI466675B (en) * | 2011-09-16 | 2015-01-01 | Univ China Medical | Pharmaceutical composition for inhibiting inflammation |
| US9241829B2 (en) | 2011-12-20 | 2016-01-26 | Abbott Medical Optics Inc. | Implantable intraocular drug delivery apparatus, system and method |
| EP2606896B1 (en) * | 2011-12-23 | 2014-08-27 | AAP Implantate AG | Sterile emulsion containing hyaluronate and glucocorticoid, and use of such emulsion in the treatment of inflammatory joint disorders |
| EP4566672A3 (en) | 2012-11-08 | 2025-08-13 | Clearside Biomedical Inc. | Methods for the treatment of ocular disease in human subjects |
| PE20151301A1 (en) | 2013-02-05 | 2015-09-16 | Purdue Pharma Lp | PHARMACEUTICAL FORMULATIONS RESISTANT TO IMPROPER HANDLING |
| CA2907765C (en) | 2013-03-21 | 2021-07-06 | Eupraxia Pharmaceuticals USA LLC | Injectable sustained release composition and method of using the same for treating inflammation in joints and pain associated therewith |
| US10494645B2 (en) | 2013-04-18 | 2019-12-03 | Fondazione Telethon | Effective delivery of large genes by dual AAV vectors |
| US9539139B2 (en) | 2013-05-03 | 2017-01-10 | Clearside Biomedical, Inc. | Apparatus and methods for ocular injection |
| CN104667287B (en) * | 2013-11-27 | 2018-02-06 | 山东博士伦福瑞达制药有限公司 | Ophthalmic composition for treating camera oculi posterior neovascularization resulting and application thereof |
| US20160310417A1 (en) * | 2013-12-20 | 2016-10-27 | Emory University | Formulations and Methods For Targeted Ocular Delivery of Therapeutic Agents |
| WO2016014408A1 (en) | 2014-07-21 | 2016-01-28 | Board Of Regents, The University Of Texas System | Formulations of intraarticular pharmaceutical agents and methods for preparing and using the same |
| ES2761558T3 (en) | 2014-09-30 | 2020-05-20 | Allergan Ind Sas | Stable hydrogel compositions including additives |
| WO2016128783A1 (en) | 2015-02-09 | 2016-08-18 | Allergan Industrie Sas | Compositions and methods for improving skin appearance |
| KR20170118105A (en) | 2015-02-13 | 2017-10-24 | 알러간 인더스트리 에스에이에스 | Implants for sculpting, enlarging or correcting facial features such as jaws |
| EP3324944A4 (en) * | 2015-07-23 | 2019-04-03 | Aerie Pharmaceuticals, Inc. | INTRAVITRANE DRUG DELIVERY SYSTEMS FOR THE TREATMENT OF OCULAR CONDITIONS |
| AU2016301103B9 (en) | 2015-07-24 | 2019-08-08 | Trimph Ip Pty Ltd | Antiseptic polymer and synthesis thereof |
| WO2017075232A1 (en) | 2015-10-27 | 2017-05-04 | Eupraxia Pharmaceuticals Inc. | Sustained release formulations of local anesthetics |
| EP3413851B1 (en) | 2016-02-10 | 2023-09-27 | Clearside Biomedical, Inc. | Packaging |
| JP2019514581A (en) | 2016-05-02 | 2019-06-06 | クリアサイド バイオメディカル,インコーポレイテッド | Systems and methods for ocular drug delivery |
| WO2018031913A1 (en) | 2016-08-12 | 2018-02-15 | Clearside Biomedical, Inc. | Devices and methods for adjusting the insertion depth of a needle for medicament delivery |
| CN109890333A (en) | 2016-09-02 | 2019-06-14 | 爱瑞制药公司 | Implantation material applicator |
| US12090294B2 (en) | 2017-05-02 | 2024-09-17 | Georgia Tech Research Corporation | Targeted drug delivery methods using a microneedle |
| IT201800007683A1 (en) | 2018-07-31 | 2020-01-31 | Altergon Sa | Synergistic cooperative compositions useful for soft tissue augmentation, drug release and related fields |
| US20210228479A1 (en) | 2020-01-29 | 2021-07-29 | Farmakeio Nutraceuticals Llc | Steroidal compositions and method of making and use |
| CA3177759A1 (en) * | 2020-05-15 | 2021-11-18 | Je Min CHAE | Methods and compositions for reducing intraocular pressure |
| AU2021328260A1 (en) * | 2020-08-17 | 2023-03-09 | Humanwell Pharmaceutical US | Long acting in-situ forming/gelling compositions |
| US20230390307A1 (en) * | 2020-10-22 | 2023-12-07 | Pfizer Inc. | Peg-free aqueous suspensions for parenteral administration of a corticosteroid |
| CN117881411A (en) * | 2021-06-01 | 2024-04-12 | 艾迪雅生物有限责任公司 | Extended release drug delivery systems for ocular drugs and methods of use |
Citations (194)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3396081A (en) | 1965-03-17 | 1968-08-06 | Etapharm Chem Pharm Lab Ges M | Hyaluronic acid preparation and method of producing same |
| US3845770A (en) | 1972-06-05 | 1974-11-05 | Alza Corp | Osmatic dispensing device for releasing beneficial agent |
| US3916899A (en) | 1973-04-25 | 1975-11-04 | Alza Corp | Osmotic dispensing device with maximum and minimum sizes for the passageway |
| US4008864A (en) | 1974-02-18 | 1977-02-22 | Nils Gustav Yngve Torphammar | Locking mechanism for a safety belt |
| US4014335A (en) | 1975-04-21 | 1977-03-29 | Alza Corporation | Ocular drug delivery device |
| US4052505A (en) | 1975-05-30 | 1977-10-04 | Alza Corporation | Ocular therapeutic system manufactured from copolymer |
| US4057619A (en) | 1975-06-30 | 1977-11-08 | Alza Corporation | Ocular therapeutic system with selected membranes for administering ophthalmic drug |
| US4063064A (en) | 1976-02-23 | 1977-12-13 | Coherent Radiation | Apparatus for tracking moving workpiece by a laser beam |
| US4088864A (en) | 1974-11-18 | 1978-05-09 | Alza Corporation | Process for forming outlet passageways in pills using a laser |
| US4144317A (en) | 1975-05-30 | 1979-03-13 | Alza Corporation | Device consisting of copolymer having acetoxy groups for delivering drugs |
| US4158005A (en) | 1975-02-10 | 1979-06-12 | Interx Research Corporation | Intermediates useful in the synthesis of optically active m-acyloxy-α-[(methylamino)methyl]benzyl alcohols |
| US4186184A (en) | 1977-12-27 | 1980-01-29 | Alza Corporation | Selective administration of drug with ocular therapeutic system |
| US4190642A (en) | 1978-04-17 | 1980-02-26 | Alza Corporation | Ocular therapeutic system for dispensing a medication formulation |
| US4200098A (en) | 1978-10-23 | 1980-04-29 | Alza Corporation | Osmotic system with distribution zone for dispensing beneficial agent |
| US4281654A (en) | 1980-04-07 | 1981-08-04 | Alza Corporation | Drug delivery system for controlled ocular therapy |
| US4285987A (en) | 1978-10-23 | 1981-08-25 | Alza Corporation | Process for manufacturing device with dispersion zone |
| US4303637A (en) | 1980-04-04 | 1981-12-01 | Alza Corporation | Medication indicated for ocular hypertension |
| US4304765A (en) | 1980-10-14 | 1981-12-08 | Alza Corporation | Ocular insert housing steroid in two different therapeutic forms |
| US4327725A (en) | 1980-11-25 | 1982-05-04 | Alza Corporation | Osmotic device with hydrogel driving member |
| US4383992A (en) | 1982-02-08 | 1983-05-17 | Lipari John M | Water-soluble steroid compounds |
| US4396625A (en) | 1980-05-13 | 1983-08-02 | Sumitomo Chemical Company, Limited | Treatment of glaucoma or ocular hypertension and ophthalmic composition |
| US4425346A (en) | 1980-08-01 | 1984-01-10 | Smith And Nephew Associated Companies Limited | Pharmaceutical compositions |
| US4474451A (en) | 1982-02-19 | 1984-10-02 | Olympus Optical Co., Ltd. | Diaphragm control circuit for TTL automatic electronic flash |
| US4478818A (en) | 1982-12-27 | 1984-10-23 | Alza Corporation | Ocular preparation housing steroid in two different therapeutic forms |
| US4494274A (en) | 1982-05-28 | 1985-01-22 | Thurlow Heida L | Cookware with covers having metal handles |
| US4521210A (en) | 1982-12-27 | 1985-06-04 | Wong Vernon G | Eye implant for relieving glaucoma, and device and method for use therewith |
| US4599353A (en) | 1982-05-03 | 1986-07-08 | The Trustees Of Columbia University In The City Of New York | Use of eicosanoids and their derivatives for treatment of ocular hypertension and glaucoma |
| US4636524A (en) | 1984-12-06 | 1987-01-13 | Biomatrix, Inc. | Cross-linked gels of hyaluronic acid and products containing such gels |
| US4649151A (en) | 1982-09-27 | 1987-03-10 | Health Research, Inc. | Drugs comprising porphyrins |
| US4656186A (en) | 1985-04-30 | 1987-04-07 | Nippon Petrochemicals Co., Ltd. | Tetrapyrrole therapeutic agents |
| US4668506A (en) | 1985-08-16 | 1987-05-26 | Bausch & Lomb Incorporated | Sustained-release formulation containing and amino acid polymer |
| US4675338A (en) | 1984-07-18 | 1987-06-23 | Nippon Petrochemicals Co., Ltd. | Tetrapyrrole therapeutic agents |
| US4693885A (en) | 1984-07-18 | 1987-09-15 | Nippon Petrochemicals Co., Ltd. | Tetrapyrrole therapeutic agents |
| US4712500A (en) | 1985-02-21 | 1987-12-15 | Nirvana Espar Systems S.A. | Mast for sailboat |
| US4713448A (en) | 1985-03-12 | 1987-12-15 | Biomatrix, Inc. | Chemically modified hyaluronic acid preparation and method of recovery thereof from animal tissues |
| US4727064A (en) | 1984-04-25 | 1988-02-23 | The United States Of America As Represented By The Department Of Health And Human Services | Pharmaceutical preparations containing cyclodextrin derivatives |
| US4853224A (en) | 1987-12-22 | 1989-08-01 | Visionex | Biodegradable ocular implants |
| US4863457A (en) | 1986-11-24 | 1989-09-05 | Lee David A | Drug delivery device |
| US4865846A (en) | 1988-06-03 | 1989-09-12 | Kaufman Herbert E | Drug delivery system |
| US4920104A (en) | 1988-05-16 | 1990-04-24 | Medchem Products, Inc. | Sodium hyaluronate composition |
| US4935498A (en) | 1989-03-06 | 1990-06-19 | Board Of Regents, The University Of Texas System | Expanded porphyrins: large porphyrin-like tripyrroledimethine-derived macrocycles |
| US4941874A (en) | 1987-08-11 | 1990-07-17 | Hoechst Aktiengesellschaft | Device for the administration of implants |
| US4959217A (en) | 1986-05-22 | 1990-09-25 | Syntex (U.S.A.) Inc. | Delayed/sustained release of macromolecules |
| US4968715A (en) | 1988-07-06 | 1990-11-06 | Health Research, Inc. | Use of purified hematoporphyrin trimers in photodynamic therapy |
| US4981871A (en) | 1987-05-15 | 1991-01-01 | Abelson Mark B | Treatment of ocular hypertension with class I calcium channel blocking agents |
| US4997652A (en) | 1987-12-22 | 1991-03-05 | Visionex | Biodegradable ocular implants |
| US5002962A (en) | 1988-07-20 | 1991-03-26 | Health Research, Inc. | Photosensitizing agents |
| US5017579A (en) | 1986-02-14 | 1991-05-21 | Sanofi | Use of aminoalkoxyphenyl derivatives for reducing and/or controlling excessive intraocular pressure |
| US5019400A (en) | 1989-05-01 | 1991-05-28 | Enzytech, Inc. | Very low temperature casting of controlled release microspheres |
| US5034413A (en) | 1989-07-27 | 1991-07-23 | Allergan, Inc. | Intraocular pressure reducing 9,11-diacyl prostaglandins |
| US5075115A (en) | 1990-04-02 | 1991-12-24 | Fmc Corporation | Process for polymerizing poly(lactic acid) |
| US5077049A (en) | 1989-07-24 | 1991-12-31 | Vipont Pharmaceutical, Inc. | Biodegradable system for regenerating the periodontium |
| US5089509A (en) | 1988-09-15 | 1992-02-18 | Allergan, Inc. | Disubstituted acetylenes bearing heteroaromatic and heterobicyclic groups having retinoid like activity |
| US5093349A (en) | 1988-07-20 | 1992-03-03 | Health Research Inc. | Photosensitizing agents |
| US5098443A (en) | 1989-03-23 | 1992-03-24 | University Of Miami | Method of implanting intraocular and intraorbital implantable devices for the controlled release of pharmacological agents |
| US5099013A (en) | 1985-03-12 | 1992-03-24 | Biomatrix, Inc, | Hylan preparation and method of recovery thereof from animal tissues |
| US5100431A (en) | 1990-09-27 | 1992-03-31 | Allergan, Inc. | Single stitch suture needle and method |
| US5106615A (en) | 1986-10-14 | 1992-04-21 | Shabtay Dikstein | Eyedrops having non-newtonian rheological properties |
| EP0488401A1 (en) | 1990-11-30 | 1992-06-03 | Senju Pharmaceutical Co., Ltd. | A controlled-release pharmaceutical preparation for intra-ocular implant |
| US5143724A (en) | 1990-07-09 | 1992-09-01 | Biomatrix, Inc. | Biocompatible viscoelastic gel slurries, their preparation and use |
| US5164188A (en) | 1989-11-22 | 1992-11-17 | Visionex, Inc. | Biodegradable ocular implants |
| US5166331A (en) | 1983-10-10 | 1992-11-24 | Fidia, S.P.A. | Hyaluronics acid fractions, methods for the preparation thereof, and pharmaceutical compositions containing same |
| US5169638A (en) | 1991-10-23 | 1992-12-08 | E. R. Squibb & Sons, Inc. | Buoyant controlled release powder formulation |
| US5171741A (en) | 1989-04-21 | 1992-12-15 | Health Research, Inc. | Bacteriochlorophyll-a derivatives useful in photodynamic therapy |
| US5173504A (en) | 1989-04-21 | 1992-12-22 | Health Research, Inc. | Bacteriochlorophyll-a derivatives useful in photodynamic therapy |
| US5190966A (en) | 1988-07-06 | 1993-03-02 | Health Research, Inc. | Purified hematoporphyrin dimers and trimers useful in photodynamic therapy |
| US5198460A (en) | 1988-07-20 | 1993-03-30 | Health Research Inc. | Pyropheophorbides and their use in photodynamic therapy |
| US5209926A (en) | 1990-06-12 | 1993-05-11 | Insite Vision Incorporated | Aminosteroids for ophthalmic use |
| US5256408A (en) | 1990-06-12 | 1993-10-26 | Insite Vision Incorporated | Aminosteroids for ophthalmic use |
| US5268178A (en) | 1989-09-25 | 1993-12-07 | The Board Of Regents, The University Of Texas System | Biodegradable antibiotic implants and methods of their use in treating and preventing infections |
| EP0197718B1 (en) | 1985-04-05 | 1993-12-15 | FIDIA S.p.A. | New medicaments for topical use |
| EP0364417B1 (en) | 1988-09-06 | 1994-02-09 | Pharmacia AB | Prostaglandin derivatives for the treatment of glaucoma or ocular hypertension |
| US5300114A (en) | 1992-05-04 | 1994-04-05 | Allergan, Inc. | Subconjunctival implants for ocular drug delivery |
| US5324519A (en) | 1989-07-24 | 1994-06-28 | Atrix Laboratories, Inc. | Biodegradable polymer composition |
| US5324718A (en) | 1992-07-14 | 1994-06-28 | Thorsteinn Loftsson | Cyclodextrin/drug complexation |
| US5332582A (en) | 1990-06-12 | 1994-07-26 | Insite Vision Incorporated | Stabilization of aminosteroids for topical ophthalmic and other applications |
| US5356629A (en) | 1991-07-12 | 1994-10-18 | United States Surgical Corporation | Composition for effecting bone repair |
| CA1333770C (en) | 1987-10-09 | 1995-01-03 | Herbert Stricker | Implantable, biodegradable system for releasing active substance |
| US5378475A (en) | 1991-02-21 | 1995-01-03 | University Of Kentucky Research Foundation | Sustained release drug delivery devices |
| US5385887A (en) | 1993-09-10 | 1995-01-31 | Genetics Institute, Inc. | Formulations for delivery of osteogenic proteins |
| WO1995013765A1 (en) | 1993-11-15 | 1995-05-26 | Oculex Pharmaceuticals, Inc. | Biocompatible ocular implants |
| US5427778A (en) | 1987-09-18 | 1995-06-27 | Ethicon, Inc. | Gel formulations containing growth factors and acrylamide polymer |
| US5438071A (en) | 1992-04-27 | 1995-08-01 | American Cyanamid Company | Stable porfimer sodium compositions and methods for their manufacture |
| US5466233A (en) | 1994-04-25 | 1995-11-14 | Escalon Ophthalmics, Inc. | Tack for intraocular drug delivery and method for inserting and removing same |
| US5487897A (en) | 1989-07-24 | 1996-01-30 | Atrix Laboratories, Inc. | Biodegradable implant precursor |
| US5494901A (en) | 1993-01-05 | 1996-02-27 | Javitt; Jonathan C. | Topical compositions for the eye comprising a β-cyclodextrin derivative and a therapeutic agent |
| US5504074A (en) | 1993-08-06 | 1996-04-02 | Children's Medical Center Corporation | Estrogenic compounds as anti-angiogenic agents |
| US5516522A (en) | 1994-03-14 | 1996-05-14 | Board Of Supervisors Of Louisiana State University | Biodegradable porous device for long-term drug delivery with constant rate release and method of making the same |
| US5552160A (en) | 1991-01-25 | 1996-09-03 | Nanosystems L.L.C. | Surface modified NSAID nanoparticles |
| US5565188A (en) | 1995-02-24 | 1996-10-15 | Nanosystems L.L.C. | Polyalkylene block copolymers as surface modifiers for nanoparticles |
| US5576311A (en) | 1994-11-30 | 1996-11-19 | Pharmos Corporation | Cyclodextrins as suspending agents for pharmaceutical suspensions |
| WO1996038174A1 (en) | 1995-06-02 | 1996-12-05 | Oculex Pharmaceuticals, Inc. | Improved formulation for controlled release of drugs by combining hydrophilic and hydrophobic agents |
| US5587479A (en) | 1992-04-09 | 1996-12-24 | Rotta Research Laboratorium S.P.A. | Basic derivatives of glutamic acid and aspartic acid as gastrin or cholecystokinin antagonists |
| US5587371A (en) | 1992-01-21 | 1996-12-24 | Pharmacyclics, Inc. | Texaphyrin-oligonucleotide conjugates |
| US5597897A (en) | 1991-06-21 | 1997-01-28 | Genetics Institute, Inc. | Pharmaceutical formulations of osteogenic proteins |
| US5656297A (en) | 1992-03-12 | 1997-08-12 | Alkermes Controlled Therapeutics, Incorporated | Modulated release from biocompatible polymers |
| US5655832A (en) | 1992-04-16 | 1997-08-12 | Tir Technologies, Inc. | Multiple wavelength light processor |
| US5688819A (en) | 1992-09-21 | 1997-11-18 | Allergan | Cyclopentane heptanoic acid, 2-cycloalkyl or arylalkyl derivatives as therapeutic agents |
| US5702716A (en) | 1988-10-03 | 1997-12-30 | Atrix Laboratories, Inc. | Polymeric compositions useful as controlled release implants |
| US5707643A (en) | 1993-02-26 | 1998-01-13 | Santen Pharmaceutical Co., Ltd. | Biodegradable scleral plug |
| US5717030A (en) | 1994-04-08 | 1998-02-10 | Atrix Laboratories, Inc. | Adjunctive polymer system for use with medical device |
| US5747061A (en) | 1993-10-25 | 1998-05-05 | Pharmos Corporation | Suspension of loteprednol etabonate for ear, eye, or nose treatment |
| US5770589A (en) | 1993-07-27 | 1998-06-23 | The University Of Sydney | Treatment of macular degeneration |
| US5776699A (en) | 1995-09-01 | 1998-07-07 | Allergan, Inc. | Method of identifying negative hormone and/or antagonist activities |
| US5780044A (en) | 1994-04-08 | 1998-07-14 | Atrix Laboratories, Inc. | Liquid delivery compositions |
| US5798349A (en) | 1994-03-14 | 1998-08-25 | The General Hospital Corporation | Use of green porphyrins to treat neovasculature in the eye |
| US5824074A (en) | 1994-02-03 | 1998-10-20 | Koch; Hans-Reinhard | Intraoccular lens arrangement and method for correcting astigmatism |
| US5877207A (en) | 1996-03-11 | 1999-03-02 | Allergan Sales, Inc. | Synthesis and use of retinoid compounds having negative hormone and/or antagonist activities |
| US5882682A (en) | 1991-12-27 | 1999-03-16 | Merck & Co., Inc. | Controlled release simvastatin delivery device |
| US5906920A (en) | 1995-08-29 | 1999-05-25 | The Salk Institute For Biological Studies | Methods for the detection of ligands for retinoid X receptors |
| US5913884A (en) | 1996-09-19 | 1999-06-22 | The General Hospital Corporation | Inhibition of fibrosis by photodynamic therapy |
| US5919970A (en) | 1997-04-24 | 1999-07-06 | Allergan Sales, Inc. | Substituted diaryl or diheteroaryl methanes, ethers and amines having retinoid agonist, antagonist or inverse agonist type biological activity |
| US5922773A (en) | 1992-12-04 | 1999-07-13 | The Children's Medical Center Corp. | Glaucoma treatment |
| US5958954A (en) | 1995-09-01 | 1999-09-28 | Allergan Sales, Inc. | Synthesis and use of retinoid compounds having negative hormone and/or antagonist activities |
| WO2000002564A1 (en) | 1998-07-10 | 2000-01-20 | The University Of Sydney | Prophylactic treatments of neovascularisation in macular degeneration |
| US6051576A (en) | 1994-01-28 | 2000-04-18 | University Of Kentucky Research Foundation | Means to achieve sustained release of synergistic drugs by conjugation |
| US6066675A (en) | 1996-09-13 | 2000-05-23 | The Regents Of The University Of California | Method for treatment of retinal diseases |
| US6074661A (en) | 1997-08-11 | 2000-06-13 | Allergan Sales, Inc. | Sterile bioerodible occular implant device with a retinoid for improved biocompatability |
| US6107347A (en) | 1990-11-30 | 2000-08-22 | Allergan | Bimodal molecular weight hyaluronate formulations and methods for using same |
| US6143314A (en) | 1998-10-28 | 2000-11-07 | Atrix Laboratories, Inc. | Controlled release liquid delivery compositions with low initial drug burst |
| US6217869B1 (en) | 1992-06-09 | 2001-04-17 | Neorx Corporation | Pretargeting methods and compounds |
| US6217895B1 (en) | 1999-03-22 | 2001-04-17 | Control Delivery Systems | Method for treating and/or preventing retinal diseases with sustained release corticosteroids |
| WO2001030323A2 (en) | 1999-10-22 | 2001-05-03 | Oculex Pharmaceuticals, Inc. | Controlled-release biocompatible ocular drug delivery implant devices and methods |
| US6251876B1 (en) | 1996-06-21 | 2001-06-26 | Fidia, S.P.A. | Autocross-linked hyaluronic acid and related pharmaceutical compositions for the treatment of arthropathies |
| US6258319B1 (en) | 1989-10-26 | 2001-07-10 | Cerus Corporation | Device and method for photoactivation |
| US6261583B1 (en) | 1998-07-28 | 2001-07-17 | Atrix Laboratories, Inc. | Moldable solid delivery system |
| US6270492B1 (en) | 1994-09-09 | 2001-08-07 | Cardiofocus, Inc. | Phototherapeutic apparatus with diffusive tip assembly |
| US6270749B1 (en) | 1996-12-11 | 2001-08-07 | Pharmacyclics, Inc. | Use of Texaphyrin in ocular diagnosis and therapy |
| US6271220B1 (en) | 1998-03-11 | 2001-08-07 | Allergan Sales, Inc. | Anti-angiogenic agents |
| US6271216B1 (en) | 1989-07-24 | 2001-08-07 | Allergan | Stable solution of hyaluronate in a balanced salt medium |
| US6274614B1 (en) | 1997-02-11 | 2001-08-14 | Qlt Inc. | Methods, compositions and articles for reducing or preventing the effects of inflammation |
| WO2001058240A2 (en) | 2000-02-10 | 2001-08-16 | Massachusetts Eye And Ear Infirmary | Photodynamic therapy for treating conditions of the eye |
| US6290713B1 (en) | 1999-08-24 | 2001-09-18 | Thomas A. Russell | Flexible illuminators for phototherapy |
| US6294361B1 (en) | 1990-05-15 | 2001-09-25 | New York Blood Center, Inc. | Processes for photoreactive inactivation of a virus in blood cell or coagulation factor containing compositions and use thereof for preparing compositions useful for transfusion |
| US6306426B1 (en) | 1997-08-11 | 2001-10-23 | Allergan Sales, Inc. | Implant device with a retinoid for improved biocompatibility |
| US6317616B1 (en) | 1999-09-15 | 2001-11-13 | Neil David Glossop | Method and system to facilitate image guided surgery |
| US6319273B1 (en) | 1999-12-16 | 2001-11-20 | Light Sciences Corporation | Illuminating device for treating eye disease |
| WO2002002076A2 (en) | 2000-07-05 | 2002-01-10 | Oculex Pharmaceuticals, Inc. | Methods for treating inflammation-mediated conditions of the eye |
| WO2002005815A1 (en) | 2000-07-13 | 2002-01-24 | Pharmacia & Upjohn Company | Ophthalmic formulation of a selective cyclooxygenase-2 inhibitory drug |
| US6357568B1 (en) | 2000-09-27 | 2002-03-19 | Shou Mao Chen | Structure for protecting a luggage shell |
| US6369116B1 (en) | 1995-06-02 | 2002-04-09 | Oculex Pharmaceuticals, Inc. | Composition and method for treating glaucoma |
| US6387409B1 (en) | 1998-03-30 | 2002-05-14 | Rtp Pharma Inc. | Composition and method of preparing microparticles of water-insoluble substances |
| US6395294B1 (en) | 2000-01-13 | 2002-05-28 | Gholam A. Peyman | Method of visualization of the vitreous during vitrectomy |
| WO2002043785A2 (en) | 2000-11-29 | 2002-06-06 | Oculex Pharmaceuticals, Inc. | Intraocular implants for preventing transplant rejection in the eye |
| US6403649B1 (en) | 1992-09-21 | 2002-06-11 | Allergan Sales, Inc. | Non-acidic cyclopentane heptanoic acid,2-cycloalkyl or arylalkyl derivatives as therapeutic agents |
| US6407079B1 (en) | 1985-07-03 | 2002-06-18 | Janssen Pharmaceutica N.V. | Pharmaceutical compositions containing drugs which are instable or sparingly soluble in water and methods for their preparation |
| US20020094998A1 (en) | 2000-11-01 | 2002-07-18 | Burke James A. | Methods and compositions for treatment of ocular neovascularization and neural injury |
| US6461631B1 (en) | 1999-11-16 | 2002-10-08 | Atrix Laboratories, Inc. | Biodegradable polymer composition |
| WO2002089815A2 (en) | 2001-05-07 | 2002-11-14 | Allergan, Inc. | Disinfecting and solubilizing steroid compositions |
| US6482854B1 (en) | 1999-03-25 | 2002-11-19 | Massachusetts Eye And Ear Infirmary | Glaucoma treatment |
| WO2002100437A2 (en) | 2001-06-08 | 2002-12-19 | Novartis Ag | Ophthalmic compositions comprising hyaluronic acid |
| US6497729B1 (en) | 1998-11-20 | 2002-12-24 | The University Of Connecticut | Implant coating for control of tissue/implant interactions |
| US20030060763A1 (en) | 2000-01-06 | 2003-03-27 | Penfold Philip Leslie | Guide means for intraocular injection |
| US20030069286A1 (en) | 2001-05-31 | 2003-04-10 | Bardeen Sciences Co., Llc | Hypotensive lipid and timolol compositions and methods of using same |
| US6565871B2 (en) | 1994-12-02 | 2003-05-20 | Elan Drug Delivery Ltd. | Solid dose delivery vehicle and methods of making same |
| US6565874B1 (en) | 1998-10-28 | 2003-05-20 | Atrix Laboratories | Polymeric delivery formulations of leuprolide with improved efficacy |
| US6573280B2 (en) | 1997-06-30 | 2003-06-03 | Allergan, Inc. | Calcium blockers to treat proliferative vitreoretinopathy |
| US6595945B2 (en) | 2001-01-09 | 2003-07-22 | J. David Brown | Glaucoma treatment device and method |
| US20030171320A1 (en) | 2001-11-09 | 2003-09-11 | Guyer David R. | Methods for treating ocular neovascular diseases |
| US6645945B1 (en) | 1996-03-05 | 2003-11-11 | Depuy Acromed, Inc. | Method of treating diseased, injured or abnormal cartilage with hyaluronic acid and growth factors |
| US20030211123A1 (en) | 2002-05-09 | 2003-11-13 | Shukla Atul J. | Vehicles for delivery of biologically active substances |
| US20030225152A1 (en) | 2001-09-27 | 2003-12-04 | Andrews Steven W. | 3-(Arylamino)methylene-1, 3-dihydro-2h-indol-2-ones as kinase inhibitors |
| US20040054374A1 (en) | 2002-09-18 | 2004-03-18 | David Weber | Methods and apparatus for delivery of ocular implants |
| US6713081B2 (en) | 2001-03-15 | 2004-03-30 | The United States Of America As Represented By The Department Of Health And Human Services | Ocular therapeutic agent delivery devices and methods for making and using such devices |
| US6713268B2 (en) | 2001-06-26 | 2004-03-30 | Allergan, Inc. | Methods of identifying ocular hypotensive compounds having reduced hyperpigmentation |
| US6723353B2 (en) | 1998-09-02 | 2004-04-20 | Allergan, Inc. | Preserved cyclodextrin-containing compositions |
| US20040077562A1 (en) | 2000-11-15 | 2004-04-22 | Chandavarkar Mohan A. | Combination drug |
| US20040137059A1 (en) | 2003-01-09 | 2004-07-15 | Thierry Nivaggioli | Biodegradable ocular implant |
| US20040152664A1 (en) | 1998-09-02 | 2004-08-05 | Allergan, Inc. | Prednisolone compositions |
| WO2004069280A1 (en) | 2003-02-06 | 2004-08-19 | Cipla Ltd | Pharmaceutical inclusion complexes containing a steroid and optionally an antibacterial agent |
| WO2004073607A2 (en) | 2003-02-20 | 2004-09-02 | Alcon, Inc. | Use of steroids to treat ocular disorders |
| WO2004087043A2 (en) | 2003-02-21 | 2004-10-14 | Sun Pharmaceutical Industries Limited | Stable ophthalmic formulation containing an antibiotic and a corticosteroid |
| US6835202B2 (en) | 1998-07-09 | 2004-12-28 | Curelight Ltd. | Apparatus and method for high energy photodynamic therapy of acne vulgaris and seborrhea |
| US20050065137A1 (en) | 2003-09-23 | 2005-03-24 | Alcon, Inc. | Triamcinolone acetonide and anecortave acetate formulations for injection |
| US20050101582A1 (en) | 2003-11-12 | 2005-05-12 | Allergan, Inc. | Compositions and methods for treating a posterior segment of an eye |
| US20050181017A1 (en) | 2004-01-20 | 2005-08-18 | Allergan, Inc. | Compositions and methods for localized therapy of the eye |
| US20050244465A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Drug delivery systems and methods for treatment of an eye |
| US20050244464A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Hypotensive lipid-containing biodegradable intraocular implants and related methods |
| US20050244470A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants containing tyrosine kinase inhibitors and related methods |
| US20050244458A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and methods for treating ocular neuropathies |
| US20050244471A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Estradiol derivative and estratopone containing sustained release intraocular implants and related methods |
| US20050244468A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and related methods |
| US20050244461A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Controlled release drug delivery systems and methods for treatment of an eye |
| US20050244463A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and methods for treating ocular vasculopathies |
| US20050244479A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and methods for preventing retinal dysfunction |
| US20050244462A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Devices and methods for treating a mammalian eye |
| US20050244478A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Anti-excititoxic sustained release intraocular implants and related methods |
| US20050244466A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Photodynamic therapy in conjunction with intraocular implants |
| US20050250737A1 (en) | 2003-11-12 | 2005-11-10 | Allergan, Inc. | Therapeutic ophthalmic compositions containing retinal friendly excipients and related methods |
| US20060009498A1 (en) | 2004-07-12 | 2006-01-12 | Allergan, Inc. | Ophthalmic compositions and methods for treating ophthalmic conditions |
| US20060141049A1 (en) | 2003-11-12 | 2006-06-29 | Allergan, Inc. | Triamcinolone compositions for intravitreal administration to treat ocular conditions |
| US20060173060A1 (en) | 2004-04-30 | 2006-08-03 | Allergan, Inc. | Oil-in-water method for making alpha-2 agonist polymeric drug delivery systems |
| US20070298073A1 (en) | 2006-06-23 | 2007-12-27 | Allergan, Inc. | Steroid-containing sustained release intraocular implants and related methods |
| US20070298074A1 (en) | 2006-06-23 | 2007-12-27 | Allergan, Inc. | Steroid-containing sustained release intraocular implants and related methods |
Family Cites Families (8)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US621583A (en) * | 1899-03-21 | Ledger balance-indicator | ||
| US385887A (en) * | 1888-07-10 | Chables sumnbr tainter | ||
| US5128326A (en) * | 1984-12-06 | 1992-07-07 | Biomatrix, Inc. | Drug delivery systems based on hyaluronans derivatives thereof and their salts and methods of producing same |
| EP0244178A3 (en) | 1986-04-28 | 1989-02-08 | Iolab, Inc | Intraocular dosage compositions and method of use |
| EP0301660B1 (en) * | 1987-07-23 | 1992-06-03 | Koninklijke Philips Electronics N.V. | Display cell |
| US4981715A (en) * | 1989-08-10 | 1991-01-01 | Microelectronics And Computer Technology Corporation | Method of patterning electroless plated metal on a polymer substrate |
| US5285887A (en) * | 1992-11-23 | 1994-02-15 | Interroll Holding A. G. | Accumulating conveyor and control system |
| US5913970A (en) * | 1997-01-16 | 1999-06-22 | Eastman Chemical Company | Stabilized non-polymeric acetoacetate esters that promote adhesion to metallic and oxidized substrates |
-
2007
- 2007-04-27 US US11/741,366 patent/US20070224278A1/en not_active Abandoned
- 2007-07-26 US US11/828,561 patent/US8846094B2/en active Active
-
2014
- 2014-08-19 US US14/463,337 patent/US9089478B2/en not_active Expired - Lifetime
Patent Citations (220)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3396081A (en) | 1965-03-17 | 1968-08-06 | Etapharm Chem Pharm Lab Ges M | Hyaluronic acid preparation and method of producing same |
| US3845770A (en) | 1972-06-05 | 1974-11-05 | Alza Corp | Osmatic dispensing device for releasing beneficial agent |
| US3916899A (en) | 1973-04-25 | 1975-11-04 | Alza Corp | Osmotic dispensing device with maximum and minimum sizes for the passageway |
| US4008864A (en) | 1974-02-18 | 1977-02-22 | Nils Gustav Yngve Torphammar | Locking mechanism for a safety belt |
| US4088864A (en) | 1974-11-18 | 1978-05-09 | Alza Corporation | Process for forming outlet passageways in pills using a laser |
| US4158005A (en) | 1975-02-10 | 1979-06-12 | Interx Research Corporation | Intermediates useful in the synthesis of optically active m-acyloxy-α-[(methylamino)methyl]benzyl alcohols |
| US4014335A (en) | 1975-04-21 | 1977-03-29 | Alza Corporation | Ocular drug delivery device |
| US4144317A (en) | 1975-05-30 | 1979-03-13 | Alza Corporation | Device consisting of copolymer having acetoxy groups for delivering drugs |
| US4052505A (en) | 1975-05-30 | 1977-10-04 | Alza Corporation | Ocular therapeutic system manufactured from copolymer |
| US4057619A (en) | 1975-06-30 | 1977-11-08 | Alza Corporation | Ocular therapeutic system with selected membranes for administering ophthalmic drug |
| US4063064A (en) | 1976-02-23 | 1977-12-13 | Coherent Radiation | Apparatus for tracking moving workpiece by a laser beam |
| US4186184A (en) | 1977-12-27 | 1980-01-29 | Alza Corporation | Selective administration of drug with ocular therapeutic system |
| US4190642A (en) | 1978-04-17 | 1980-02-26 | Alza Corporation | Ocular therapeutic system for dispensing a medication formulation |
| US4200098A (en) | 1978-10-23 | 1980-04-29 | Alza Corporation | Osmotic system with distribution zone for dispensing beneficial agent |
| US4285987A (en) | 1978-10-23 | 1981-08-25 | Alza Corporation | Process for manufacturing device with dispersion zone |
| US4303637A (en) | 1980-04-04 | 1981-12-01 | Alza Corporation | Medication indicated for ocular hypertension |
| US4281654A (en) | 1980-04-07 | 1981-08-04 | Alza Corporation | Drug delivery system for controlled ocular therapy |
| US4396625A (en) | 1980-05-13 | 1983-08-02 | Sumitomo Chemical Company, Limited | Treatment of glaucoma or ocular hypertension and ophthalmic composition |
| US4425346A (en) | 1980-08-01 | 1984-01-10 | Smith And Nephew Associated Companies Limited | Pharmaceutical compositions |
| US4304765A (en) | 1980-10-14 | 1981-12-08 | Alza Corporation | Ocular insert housing steroid in two different therapeutic forms |
| US4327725A (en) | 1980-11-25 | 1982-05-04 | Alza Corporation | Osmotic device with hydrogel driving member |
| US4383992A (en) | 1982-02-08 | 1983-05-17 | Lipari John M | Water-soluble steroid compounds |
| US4474451A (en) | 1982-02-19 | 1984-10-02 | Olympus Optical Co., Ltd. | Diaphragm control circuit for TTL automatic electronic flash |
| US4599353A (en) | 1982-05-03 | 1986-07-08 | The Trustees Of Columbia University In The City Of New York | Use of eicosanoids and their derivatives for treatment of ocular hypertension and glaucoma |
| US4494274A (en) | 1982-05-28 | 1985-01-22 | Thurlow Heida L | Cookware with covers having metal handles |
| US5028621A (en) | 1982-09-27 | 1991-07-02 | Health Research, Inc. | Drugs comprising porphyrins |
| US4932934A (en) | 1982-09-27 | 1990-06-12 | Health Research, Inc. | Methods for treatment of tumors |
| US4866168A (en) | 1982-09-27 | 1989-09-12 | Health Research, Inc. | Hematoporphyrin derivatives and process of preparing |
| US4649151A (en) | 1982-09-27 | 1987-03-10 | Health Research, Inc. | Drugs comprising porphyrins |
| US4478818A (en) | 1982-12-27 | 1984-10-23 | Alza Corporation | Ocular preparation housing steroid in two different therapeutic forms |
| US4521210A (en) | 1982-12-27 | 1985-06-04 | Wong Vernon G | Eye implant for relieving glaucoma, and device and method for use therewith |
| US5166331A (en) | 1983-10-10 | 1992-11-24 | Fidia, S.P.A. | Hyaluronics acid fractions, methods for the preparation thereof, and pharmaceutical compositions containing same |
| US4727064A (en) | 1984-04-25 | 1988-02-23 | The United States Of America As Represented By The Department Of Health And Human Services | Pharmaceutical preparations containing cyclodextrin derivatives |
| US4675338A (en) | 1984-07-18 | 1987-06-23 | Nippon Petrochemicals Co., Ltd. | Tetrapyrrole therapeutic agents |
| US4693885A (en) | 1984-07-18 | 1987-09-15 | Nippon Petrochemicals Co., Ltd. | Tetrapyrrole therapeutic agents |
| US4636524A (en) | 1984-12-06 | 1987-01-13 | Biomatrix, Inc. | Cross-linked gels of hyaluronic acid and products containing such gels |
| US4712500A (en) | 1985-02-21 | 1987-12-15 | Nirvana Espar Systems S.A. | Mast for sailboat |
| US4713448A (en) | 1985-03-12 | 1987-12-15 | Biomatrix, Inc. | Chemically modified hyaluronic acid preparation and method of recovery thereof from animal tissues |
| US5099013A (en) | 1985-03-12 | 1992-03-24 | Biomatrix, Inc, | Hylan preparation and method of recovery thereof from animal tissues |
| EP0197718B1 (en) | 1985-04-05 | 1993-12-15 | FIDIA S.p.A. | New medicaments for topical use |
| US4656186A (en) | 1985-04-30 | 1987-04-07 | Nippon Petrochemicals Co., Ltd. | Tetrapyrrole therapeutic agents |
| US6407079B1 (en) | 1985-07-03 | 2002-06-18 | Janssen Pharmaceutica N.V. | Pharmaceutical compositions containing drugs which are instable or sparingly soluble in water and methods for their preparation |
| US4668506A (en) | 1985-08-16 | 1987-05-26 | Bausch & Lomb Incorporated | Sustained-release formulation containing and amino acid polymer |
| US5017579A (en) | 1986-02-14 | 1991-05-21 | Sanofi | Use of aminoalkoxyphenyl derivatives for reducing and/or controlling excessive intraocular pressure |
| US4959217A (en) | 1986-05-22 | 1990-09-25 | Syntex (U.S.A.) Inc. | Delayed/sustained release of macromolecules |
| US5106615A (en) | 1986-10-14 | 1992-04-21 | Shabtay Dikstein | Eyedrops having non-newtonian rheological properties |
| US4863457A (en) | 1986-11-24 | 1989-09-05 | Lee David A | Drug delivery device |
| US4981871A (en) | 1987-05-15 | 1991-01-01 | Abelson Mark B | Treatment of ocular hypertension with class I calcium channel blocking agents |
| US4941874A (en) | 1987-08-11 | 1990-07-17 | Hoechst Aktiengesellschaft | Device for the administration of implants |
| US5427778A (en) | 1987-09-18 | 1995-06-27 | Ethicon, Inc. | Gel formulations containing growth factors and acrylamide polymer |
| CA1333770C (en) | 1987-10-09 | 1995-01-03 | Herbert Stricker | Implantable, biodegradable system for releasing active substance |
| US4997652A (en) | 1987-12-22 | 1991-03-05 | Visionex | Biodegradable ocular implants |
| US4853224A (en) | 1987-12-22 | 1989-08-01 | Visionex | Biodegradable ocular implants |
| US4920104A (en) | 1988-05-16 | 1990-04-24 | Medchem Products, Inc. | Sodium hyaluronate composition |
| US4865846A (en) | 1988-06-03 | 1989-09-12 | Kaufman Herbert E | Drug delivery system |
| US4968715A (en) | 1988-07-06 | 1990-11-06 | Health Research, Inc. | Use of purified hematoporphyrin trimers in photodynamic therapy |
| US5190966A (en) | 1988-07-06 | 1993-03-02 | Health Research, Inc. | Purified hematoporphyrin dimers and trimers useful in photodynamic therapy |
| US5314905A (en) | 1988-07-20 | 1994-05-24 | Health Research, Inc. | Pyropheophorbides conjugates and their use in photodynamic therapy |
| US5093349A (en) | 1988-07-20 | 1992-03-03 | Health Research Inc. | Photosensitizing agents |
| US5002962A (en) | 1988-07-20 | 1991-03-26 | Health Research, Inc. | Photosensitizing agents |
| US5459159A (en) | 1988-07-20 | 1995-10-17 | Health Research, Inc. | Pyropheophorbides and their use in photodynamic therapy |
| US5198460A (en) | 1988-07-20 | 1993-03-30 | Health Research Inc. | Pyropheophorbides and their use in photodynamic therapy |
| EP0364417B1 (en) | 1988-09-06 | 1994-02-09 | Pharmacia AB | Prostaglandin derivatives for the treatment of glaucoma or ocular hypertension |
| US5089509A (en) | 1988-09-15 | 1992-02-18 | Allergan, Inc. | Disubstituted acetylenes bearing heteroaromatic and heterobicyclic groups having retinoid like activity |
| US5702716A (en) | 1988-10-03 | 1997-12-30 | Atrix Laboratories, Inc. | Polymeric compositions useful as controlled release implants |
| US4935498A (en) | 1989-03-06 | 1990-06-19 | Board Of Regents, The University Of Texas System | Expanded porphyrins: large porphyrin-like tripyrroledimethine-derived macrocycles |
| US5098443A (en) | 1989-03-23 | 1992-03-24 | University Of Miami | Method of implanting intraocular and intraorbital implantable devices for the controlled release of pharmacological agents |
| US5173504A (en) | 1989-04-21 | 1992-12-22 | Health Research, Inc. | Bacteriochlorophyll-a derivatives useful in photodynamic therapy |
| US5171741A (en) | 1989-04-21 | 1992-12-15 | Health Research, Inc. | Bacteriochlorophyll-a derivatives useful in photodynamic therapy |
| US5019400A (en) | 1989-05-01 | 1991-05-28 | Enzytech, Inc. | Very low temperature casting of controlled release microspheres |
| US5487897A (en) | 1989-07-24 | 1996-01-30 | Atrix Laboratories, Inc. | Biodegradable implant precursor |
| US6395293B2 (en) | 1989-07-24 | 2002-05-28 | Atrix Laboratories | Biodegradable implant precursor |
| US6271216B1 (en) | 1989-07-24 | 2001-08-07 | Allergan | Stable solution of hyaluronate in a balanced salt medium |
| US5077049A (en) | 1989-07-24 | 1991-12-31 | Vipont Pharmaceutical, Inc. | Biodegradable system for regenerating the periodontium |
| US5324519A (en) | 1989-07-24 | 1994-06-28 | Atrix Laboratories, Inc. | Biodegradable polymer composition |
| US5034413A (en) | 1989-07-27 | 1991-07-23 | Allergan, Inc. | Intraocular pressure reducing 9,11-diacyl prostaglandins |
| US5268178A (en) | 1989-09-25 | 1993-12-07 | The Board Of Regents, The University Of Texas System | Biodegradable antibiotic implants and methods of their use in treating and preventing infections |
| US6258319B1 (en) | 1989-10-26 | 2001-07-10 | Cerus Corporation | Device and method for photoactivation |
| EP0430539B1 (en) | 1989-11-22 | 1994-10-12 | Visionex, Inc. | Ocular implants |
| US5164188A (en) | 1989-11-22 | 1992-11-17 | Visionex, Inc. | Biodegradable ocular implants |
| US5075115A (en) | 1990-04-02 | 1991-12-24 | Fmc Corporation | Process for polymerizing poly(lactic acid) |
| US6294361B1 (en) | 1990-05-15 | 2001-09-25 | New York Blood Center, Inc. | Processes for photoreactive inactivation of a virus in blood cell or coagulation factor containing compositions and use thereof for preparing compositions useful for transfusion |
| US5332582A (en) | 1990-06-12 | 1994-07-26 | Insite Vision Incorporated | Stabilization of aminosteroids for topical ophthalmic and other applications |
| US5256408A (en) | 1990-06-12 | 1993-10-26 | Insite Vision Incorporated | Aminosteroids for ophthalmic use |
| US5209926A (en) | 1990-06-12 | 1993-05-11 | Insite Vision Incorporated | Aminosteroids for ophthalmic use |
| US5143724A (en) | 1990-07-09 | 1992-09-01 | Biomatrix, Inc. | Biocompatible viscoelastic gel slurries, their preparation and use |
| US5100431A (en) | 1990-09-27 | 1992-03-31 | Allergan, Inc. | Single stitch suture needle and method |
| US6107347A (en) | 1990-11-30 | 2000-08-22 | Allergan | Bimodal molecular weight hyaluronate formulations and methods for using same |
| US5501856A (en) | 1990-11-30 | 1996-03-26 | Senju Pharmaceutical Co., Ltd. | Controlled-release pharmaceutical preparation for intra-ocular implant |
| EP0488401A1 (en) | 1990-11-30 | 1992-06-03 | Senju Pharmaceutical Co., Ltd. | A controlled-release pharmaceutical preparation for intra-ocular implant |
| US5552160A (en) | 1991-01-25 | 1996-09-03 | Nanosystems L.L.C. | Surface modified NSAID nanoparticles |
| US5378475A (en) | 1991-02-21 | 1995-01-03 | University Of Kentucky Research Foundation | Sustained release drug delivery devices |
| US5597897A (en) | 1991-06-21 | 1997-01-28 | Genetics Institute, Inc. | Pharmaceutical formulations of osteogenic proteins |
| US5356629A (en) | 1991-07-12 | 1994-10-18 | United States Surgical Corporation | Composition for effecting bone repair |
| US5169638A (en) | 1991-10-23 | 1992-12-08 | E. R. Squibb & Sons, Inc. | Buoyant controlled release powder formulation |
| US5882682A (en) | 1991-12-27 | 1999-03-16 | Merck & Co., Inc. | Controlled release simvastatin delivery device |
| US5587371A (en) | 1992-01-21 | 1996-12-24 | Pharmacyclics, Inc. | Texaphyrin-oligonucleotide conjugates |
| US5656297A (en) | 1992-03-12 | 1997-08-12 | Alkermes Controlled Therapeutics, Incorporated | Modulated release from biocompatible polymers |
| US5587479A (en) | 1992-04-09 | 1996-12-24 | Rotta Research Laboratorium S.P.A. | Basic derivatives of glutamic acid and aspartic acid as gastrin or cholecystokinin antagonists |
| US5655832A (en) | 1992-04-16 | 1997-08-12 | Tir Technologies, Inc. | Multiple wavelength light processor |
| US5438071A (en) | 1992-04-27 | 1995-08-01 | American Cyanamid Company | Stable porfimer sodium compositions and methods for their manufacture |
| US5300114A (en) | 1992-05-04 | 1994-04-05 | Allergan, Inc. | Subconjunctival implants for ocular drug delivery |
| US6217869B1 (en) | 1992-06-09 | 2001-04-17 | Neorx Corporation | Pretargeting methods and compounds |
| US5324718A (en) | 1992-07-14 | 1994-06-28 | Thorsteinn Loftsson | Cyclodextrin/drug complexation |
| US6403649B1 (en) | 1992-09-21 | 2002-06-11 | Allergan Sales, Inc. | Non-acidic cyclopentane heptanoic acid,2-cycloalkyl or arylalkyl derivatives as therapeutic agents |
| US5688819A (en) | 1992-09-21 | 1997-11-18 | Allergan | Cyclopentane heptanoic acid, 2-cycloalkyl or arylalkyl derivatives as therapeutic agents |
| US5922773A (en) | 1992-12-04 | 1999-07-13 | The Children's Medical Center Corp. | Glaucoma treatment |
| US5494901A (en) | 1993-01-05 | 1996-02-27 | Javitt; Jonathan C. | Topical compositions for the eye comprising a β-cyclodextrin derivative and a therapeutic agent |
| US5707643A (en) | 1993-02-26 | 1998-01-13 | Santen Pharmaceutical Co., Ltd. | Biodegradable scleral plug |
| US5770589A (en) | 1993-07-27 | 1998-06-23 | The University Of Sydney | Treatment of macular degeneration |
| US5504074A (en) | 1993-08-06 | 1996-04-02 | Children's Medical Center Corporation | Estrogenic compounds as anti-angiogenic agents |
| US5385887A (en) | 1993-09-10 | 1995-01-31 | Genetics Institute, Inc. | Formulations for delivery of osteogenic proteins |
| US5747061A (en) | 1993-10-25 | 1998-05-05 | Pharmos Corporation | Suspension of loteprednol etabonate for ear, eye, or nose treatment |
| WO1995013765A1 (en) | 1993-11-15 | 1995-05-26 | Oculex Pharmaceuticals, Inc. | Biocompatible ocular implants |
| US5824072A (en) | 1993-11-15 | 1998-10-20 | Oculex Pharmaceuticals, Inc. | Biocompatible ocular implants |
| US5766242A (en) | 1993-11-15 | 1998-06-16 | Oculex Pharmaceuticals, Inc. | Biocompatible ocular implants |
| US5443505A (en) | 1993-11-15 | 1995-08-22 | Oculex Pharmaceuticals, Inc. | Biocompatible ocular implants |
| US6051576A (en) | 1994-01-28 | 2000-04-18 | University Of Kentucky Research Foundation | Means to achieve sustained release of synergistic drugs by conjugation |
| US5824074A (en) | 1994-02-03 | 1998-10-20 | Koch; Hans-Reinhard | Intraoccular lens arrangement and method for correcting astigmatism |
| US6225303B1 (en) | 1994-03-14 | 2001-05-01 | Massachusetts Eye And Ear Infirmary | Use of green porphyrins to treat neovasculature in the eye |
| US5516522A (en) | 1994-03-14 | 1996-05-14 | Board Of Supervisors Of Louisiana State University | Biodegradable porous device for long-term drug delivery with constant rate release and method of making the same |
| US5798349A (en) | 1994-03-14 | 1998-08-25 | The General Hospital Corporation | Use of green porphyrins to treat neovasculature in the eye |
| US5717030A (en) | 1994-04-08 | 1998-02-10 | Atrix Laboratories, Inc. | Adjunctive polymer system for use with medical device |
| US5780044A (en) | 1994-04-08 | 1998-07-14 | Atrix Laboratories, Inc. | Liquid delivery compositions |
| US5466233A (en) | 1994-04-25 | 1995-11-14 | Escalon Ophthalmics, Inc. | Tack for intraocular drug delivery and method for inserting and removing same |
| US6270492B1 (en) | 1994-09-09 | 2001-08-07 | Cardiofocus, Inc. | Phototherapeutic apparatus with diffusive tip assembly |
| US5576311A (en) | 1994-11-30 | 1996-11-19 | Pharmos Corporation | Cyclodextrins as suspending agents for pharmaceutical suspensions |
| US6565871B2 (en) | 1994-12-02 | 2003-05-20 | Elan Drug Delivery Ltd. | Solid dose delivery vehicle and methods of making same |
| US5565188A (en) | 1995-02-24 | 1996-10-15 | Nanosystems L.L.C. | Polyalkylene block copolymers as surface modifiers for nanoparticles |
| US20030095995A1 (en) | 1995-06-02 | 2003-05-22 | Vernon Wong | Formulation for controlled release of drugs by combining hydrophilic and hydrophobic agents |
| WO1996038174A1 (en) | 1995-06-02 | 1996-12-05 | Oculex Pharmaceuticals, Inc. | Improved formulation for controlled release of drugs by combining hydrophilic and hydrophobic agents |
| US6369116B1 (en) | 1995-06-02 | 2002-04-09 | Oculex Pharmaceuticals, Inc. | Composition and method for treating glaucoma |
| US5869079A (en) | 1995-06-02 | 1999-02-09 | Oculex Pharmaceuticals, Inc. | Formulation for controlled release of drugs by combining hydrophilic and hydrophobic agents |
| US5906920A (en) | 1995-08-29 | 1999-05-25 | The Salk Institute For Biological Studies | Methods for the detection of ligands for retinoid X receptors |
| US5958954A (en) | 1995-09-01 | 1999-09-28 | Allergan Sales, Inc. | Synthesis and use of retinoid compounds having negative hormone and/or antagonist activities |
| US5776699A (en) | 1995-09-01 | 1998-07-07 | Allergan, Inc. | Method of identifying negative hormone and/or antagonist activities |
| US6645945B1 (en) | 1996-03-05 | 2003-11-11 | Depuy Acromed, Inc. | Method of treating diseased, injured or abnormal cartilage with hyaluronic acid and growth factors |
| US5877207A (en) | 1996-03-11 | 1999-03-02 | Allergan Sales, Inc. | Synthesis and use of retinoid compounds having negative hormone and/or antagonist activities |
| US6251876B1 (en) | 1996-06-21 | 2001-06-26 | Fidia, S.P.A. | Autocross-linked hyaluronic acid and related pharmaceutical compositions for the treatment of arthropathies |
| US6066675A (en) | 1996-09-13 | 2000-05-23 | The Regents Of The University Of California | Method for treatment of retinal diseases |
| US5913884A (en) | 1996-09-19 | 1999-06-22 | The General Hospital Corporation | Inhibition of fibrosis by photodynamic therapy |
| US6270749B1 (en) | 1996-12-11 | 2001-08-07 | Pharmacyclics, Inc. | Use of Texaphyrin in ocular diagnosis and therapy |
| US6274614B1 (en) | 1997-02-11 | 2001-08-14 | Qlt Inc. | Methods, compositions and articles for reducing or preventing the effects of inflammation |
| US5919970A (en) | 1997-04-24 | 1999-07-06 | Allergan Sales, Inc. | Substituted diaryl or diheteroaryl methanes, ethers and amines having retinoid agonist, antagonist or inverse agonist type biological activity |
| US6573280B2 (en) | 1997-06-30 | 2003-06-03 | Allergan, Inc. | Calcium blockers to treat proliferative vitreoretinopathy |
| US6537568B2 (en) | 1997-08-11 | 2003-03-25 | Allergan, Inc. | Implant device with a retinoid for improved biocompatibility |
| US6306426B1 (en) | 1997-08-11 | 2001-10-23 | Allergan Sales, Inc. | Implant device with a retinoid for improved biocompatibility |
| US6074661A (en) | 1997-08-11 | 2000-06-13 | Allergan Sales, Inc. | Sterile bioerodible occular implant device with a retinoid for improved biocompatability |
| US6455062B1 (en) | 1997-08-11 | 2002-09-24 | Allergan, Inc. | Implant device with a retinoid for improved biocompatibility |
| US6271220B1 (en) | 1998-03-11 | 2001-08-07 | Allergan Sales, Inc. | Anti-angiogenic agents |
| US6387409B1 (en) | 1998-03-30 | 2002-05-14 | Rtp Pharma Inc. | Composition and method of preparing microparticles of water-insoluble substances |
| US6835202B2 (en) | 1998-07-09 | 2004-12-28 | Curelight Ltd. | Apparatus and method for high energy photodynamic therapy of acne vulgaris and seborrhea |
| WO2000002564A1 (en) | 1998-07-10 | 2000-01-20 | The University Of Sydney | Prophylactic treatments of neovascularisation in macular degeneration |
| US6261583B1 (en) | 1998-07-28 | 2001-07-17 | Atrix Laboratories, Inc. | Moldable solid delivery system |
| US6723353B2 (en) | 1998-09-02 | 2004-04-20 | Allergan, Inc. | Preserved cyclodextrin-containing compositions |
| US20040152664A1 (en) | 1998-09-02 | 2004-08-05 | Allergan, Inc. | Prednisolone compositions |
| US6565874B1 (en) | 1998-10-28 | 2003-05-20 | Atrix Laboratories | Polymeric delivery formulations of leuprolide with improved efficacy |
| US6143314A (en) | 1998-10-28 | 2000-11-07 | Atrix Laboratories, Inc. | Controlled release liquid delivery compositions with low initial drug burst |
| US6497729B1 (en) | 1998-11-20 | 2002-12-24 | The University Of Connecticut | Implant coating for control of tissue/implant interactions |
| US6548078B2 (en) | 1999-03-22 | 2003-04-15 | Control Delivery Systems | Method for treating and/or preventing retinal diseases with sustained release corticosteroids |
| US6217895B1 (en) | 1999-03-22 | 2001-04-17 | Control Delivery Systems | Method for treating and/or preventing retinal diseases with sustained release corticosteroids |
| US6482854B1 (en) | 1999-03-25 | 2002-11-19 | Massachusetts Eye And Ear Infirmary | Glaucoma treatment |
| US6290713B1 (en) | 1999-08-24 | 2001-09-18 | Thomas A. Russell | Flexible illuminators for phototherapy |
| US6317616B1 (en) | 1999-09-15 | 2001-11-13 | Neil David Glossop | Method and system to facilitate image guided surgery |
| WO2001030323A2 (en) | 1999-10-22 | 2001-05-03 | Oculex Pharmaceuticals, Inc. | Controlled-release biocompatible ocular drug delivery implant devices and methods |
| US6331313B1 (en) | 1999-10-22 | 2001-12-18 | Oculex Pharmaceticals, Inc. | Controlled-release biocompatible ocular drug delivery implant devices and methods |
| US6461631B1 (en) | 1999-11-16 | 2002-10-08 | Atrix Laboratories, Inc. | Biodegradable polymer composition |
| US6319273B1 (en) | 1999-12-16 | 2001-11-20 | Light Sciences Corporation | Illuminating device for treating eye disease |
| US20030060763A1 (en) | 2000-01-06 | 2003-03-27 | Penfold Philip Leslie | Guide means for intraocular injection |
| US6395294B1 (en) | 2000-01-13 | 2002-05-28 | Gholam A. Peyman | Method of visualization of the vitreous during vitrectomy |
| US7125542B2 (en) | 2000-02-10 | 2006-10-24 | Massachusetts Eye And Ear Infirmary | Methods and compositions for treating conditions of the eye |
| WO2001058240A2 (en) | 2000-02-10 | 2001-08-16 | Massachusetts Eye And Ear Infirmary | Photodynamic therapy for treating conditions of the eye |
| WO2002002076A2 (en) | 2000-07-05 | 2002-01-10 | Oculex Pharmaceuticals, Inc. | Methods for treating inflammation-mediated conditions of the eye |
| US6726918B1 (en) | 2000-07-05 | 2004-04-27 | Oculex Pharmaceuticals, Inc. | Methods for treating inflammation-mediated conditions of the eye |
| WO2002005815A1 (en) | 2000-07-13 | 2002-01-24 | Pharmacia & Upjohn Company | Ophthalmic formulation of a selective cyclooxygenase-2 inhibitory drug |
| US6357568B1 (en) | 2000-09-27 | 2002-03-19 | Shou Mao Chen | Structure for protecting a luggage shell |
| US20020094998A1 (en) | 2000-11-01 | 2002-07-18 | Burke James A. | Methods and compositions for treatment of ocular neovascularization and neural injury |
| US20040077562A1 (en) | 2000-11-15 | 2004-04-22 | Chandavarkar Mohan A. | Combination drug |
| WO2002043785A2 (en) | 2000-11-29 | 2002-06-06 | Oculex Pharmaceuticals, Inc. | Intraocular implants for preventing transplant rejection in the eye |
| US6699493B2 (en) | 2000-11-29 | 2004-03-02 | Oculex Pharmaceuticals, Inc. | Method for reducing or preventing transplant rejection in the eye and intraocular implants for use therefor |
| US6595945B2 (en) | 2001-01-09 | 2003-07-22 | J. David Brown | Glaucoma treatment device and method |
| US6713081B2 (en) | 2001-03-15 | 2004-03-30 | The United States Of America As Represented By The Department Of Health And Human Services | Ocular therapeutic agent delivery devices and methods for making and using such devices |
| US20020198174A1 (en) | 2001-05-07 | 2002-12-26 | Allergan Sales, Inc. | Disinfecting and solubilizing steroid compositions |
| WO2002089815A2 (en) | 2001-05-07 | 2002-11-14 | Allergan, Inc. | Disinfecting and solubilizing steroid compositions |
| US20030069286A1 (en) | 2001-05-31 | 2003-04-10 | Bardeen Sciences Co., Llc | Hypotensive lipid and timolol compositions and methods of using same |
| WO2002100437A2 (en) | 2001-06-08 | 2002-12-19 | Novartis Ag | Ophthalmic compositions comprising hyaluronic acid |
| US6713268B2 (en) | 2001-06-26 | 2004-03-30 | Allergan, Inc. | Methods of identifying ocular hypotensive compounds having reduced hyperpigmentation |
| US6765012B2 (en) | 2001-09-27 | 2004-07-20 | Allergan, Inc. | 3-(Arylamino)methylene-1,3-dihydro-2H-indol-2-ones as kinase inhibitors |
| US20030225152A1 (en) | 2001-09-27 | 2003-12-04 | Andrews Steven W. | 3-(Arylamino)methylene-1, 3-dihydro-2h-indol-2-ones as kinase inhibitors |
| US20030171320A1 (en) | 2001-11-09 | 2003-09-11 | Guyer David R. | Methods for treating ocular neovascular diseases |
| US20030211123A1 (en) | 2002-05-09 | 2003-11-13 | Shukla Atul J. | Vehicles for delivery of biologically active substances |
| US20040054374A1 (en) | 2002-09-18 | 2004-03-18 | David Weber | Methods and apparatus for delivery of ocular implants |
| US6899717B2 (en) | 2002-09-18 | 2005-05-31 | Allergan, Inc. | Methods and apparatus for delivery of ocular implants |
| US20040137059A1 (en) | 2003-01-09 | 2004-07-15 | Thierry Nivaggioli | Biodegradable ocular implant |
| WO2004069280A1 (en) | 2003-02-06 | 2004-08-19 | Cipla Ltd | Pharmaceutical inclusion complexes containing a steroid and optionally an antibacterial agent |
| WO2004073607A2 (en) | 2003-02-20 | 2004-09-02 | Alcon, Inc. | Use of steroids to treat ocular disorders |
| WO2004087043A2 (en) | 2003-02-21 | 2004-10-14 | Sun Pharmaceutical Industries Limited | Stable ophthalmic formulation containing an antibiotic and a corticosteroid |
| US20050065137A1 (en) | 2003-09-23 | 2005-03-24 | Alcon, Inc. | Triamcinolone acetonide and anecortave acetate formulations for injection |
| US20050250737A1 (en) | 2003-11-12 | 2005-11-10 | Allergan, Inc. | Therapeutic ophthalmic compositions containing retinal friendly excipients and related methods |
| US20050101582A1 (en) | 2003-11-12 | 2005-05-12 | Allergan, Inc. | Compositions and methods for treating a posterior segment of an eye |
| US20060141049A1 (en) | 2003-11-12 | 2006-06-29 | Allergan, Inc. | Triamcinolone compositions for intravitreal administration to treat ocular conditions |
| US20050181017A1 (en) | 2004-01-20 | 2005-08-18 | Allergan, Inc. | Compositions and methods for localized therapy of the eye |
| US20050244462A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Devices and methods for treating a mammalian eye |
| US20050244466A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Photodynamic therapy in conjunction with intraocular implants |
| US20050244468A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and related methods |
| US20050244461A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Controlled release drug delivery systems and methods for treatment of an eye |
| US20050244463A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and methods for treating ocular vasculopathies |
| US20050244474A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Steroid-containing sustained release intraocular implants and related methods |
| US20050244479A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and methods for preventing retinal dysfunction |
| US20050244465A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Drug delivery systems and methods for treatment of an eye |
| US20050244478A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Anti-excititoxic sustained release intraocular implants and related methods |
| US20050244471A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Estradiol derivative and estratopone containing sustained release intraocular implants and related methods |
| US20050244458A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants and methods for treating ocular neuropathies |
| WO2005110380A1 (en) | 2004-04-30 | 2005-11-24 | Allergan, Inc. | Sustained release intraocular implants comprising a beta adrenergic receptor antagonist and methods for treating ocular neuropathies |
| US20050244464A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Hypotensive lipid-containing biodegradable intraocular implants and related methods |
| US20050244470A1 (en) | 2004-04-30 | 2005-11-03 | Allergan, Inc. | Sustained release intraocular implants containing tyrosine kinase inhibitors and related methods |
| US20060173060A1 (en) | 2004-04-30 | 2006-08-03 | Allergan, Inc. | Oil-in-water method for making alpha-2 agonist polymeric drug delivery systems |
| US20060009498A1 (en) | 2004-07-12 | 2006-01-12 | Allergan, Inc. | Ophthalmic compositions and methods for treating ophthalmic conditions |
| US20070298073A1 (en) | 2006-06-23 | 2007-12-27 | Allergan, Inc. | Steroid-containing sustained release intraocular implants and related methods |
| US20070298074A1 (en) | 2006-06-23 | 2007-12-27 | Allergan, Inc. | Steroid-containing sustained release intraocular implants and related methods |
Non-Patent Citations (146)
| Title |
|---|
| "Lumigan found effective in early phase 3", Ocular Surgery News, Mar. 2001; 19(5):1,35. |
| "Lumigan®: a new ocular hypotensive agent for achieving target intraocular pressures," Acta Ophthalmologica Scandinavica, Scientific Abstracts, 2002; 80(4):457. |
| "Tazarotene", Drugs Future, 2003; 28(2):208-209. Annual Update 2003: Dermatologic Drugs. |
| Adams, Mark, An Analysis of Clinical Studies of the Use of Crosslinked Hyaluronan, Hylan, in the Treatment of Osteoarthritis, The Journal of Rheumatology, 1993, 16-18, 20 (39). |
| ALPHAGAN® P, Product Information. |
| Anderson, L.C. et al., An Injectable Substained Release Fertility Control System, Contraception, 1976;,13:375-384. |
| Antcliff R., et al Marshall J., The pathogenesis of edema in diabetic maculopathy, Semin Ophthalmol 1999; 14:223-232. |
| Armaly M., Statistical attributes of the steroid hypertensive response in the clinically normal eye, Invest Ophthalmol Vis Sci 1965; 4:187-197. |
| Audren, F. et al., Pharmacokinetic-Pharmacodynamic modeling of the effect of Triamcinolone Acetonide on Central Macular Thickness in Patients with Diabetic Macular Edema, Inv Ophth & Vis Sci, 45(10); 3435-3441: Oct. 2004. |
| Aukunuru et al., In Vitro Delivery of Nano- and Micro-Particles to Human Retinal Pigment Epithelial (ARPE-19) Cells, Drug Delivery Technologies, 2002; 2(2):50-57. |
| Baker R., Controlled Release of Biologically Active Agents, A Wiley-Interscience Publication, 1987; 73-75. |
| Becker B,. Intraocular pressure response to topical corticosteroid, Invest Ophthalmol Vis Sci 1965; 4:198-205. |
| Beer P. et al., Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection, Opthal 110(4); 681-686: Apr. 2003. |
| Bito L.Z., Glaucoma: Applied Pharmacology in the Medical Treatment, Drance, S.M. and Neufled, A.H. Eds., New York, Grune & Stratton, 1984; 477-505. |
| Bito L.Z., Prostaglandins: Old Concepts and New Perspectives, Archives of Ophthalmology, 1987; 105:1036-1039. |
| Bito, L.Z., Biological protection with prostaglandins, Cohen, M.M., ed., Boca Raton, Fla., CRC Press Inc., 1985; 31-252. |
| Bodor, N. et al., A Comparison of Intraocular Pressure Elevating Activity of Loteprednol Etabonate and Dexamethasone in Rabbits, Current Eye Research, 1992; 11:525-530. |
| Brubaker, Mechanism of Action of Bimatoprost (Lumigan(TM)), Survey of Ophthalmology, 2001; 45(Suppl 4):S347-S351. |
| Brubaker, Mechanism of Action of Bimatoprost (Lumigan™), Survey of Ophthalmology, 2001; 45(Suppl 4):S347-S351. |
| Busse et al., Tyrosine kinase inhibitors: rationale, mechanisms of action, and implications for drug resistance, Seminars in Oncology, 2001; 28(suppl 16):47-55. |
| Butcher J. et al., Bilateral cataracts and glaucoma induced by long term use of steroid eye drops. BMJ 1994; 309-343. |
| Capozzi, Angelo et al, Distant Migration of Silicone Gel From a Ruptured Breast Implant, Silicone Gel Migration, 1978, 302-3, 62 (2). |
| Challa J. et al., Exudative macular degeneration and intravitreal triamcinolone: 18 month follow up, Aust NZ J Ophthalmol 1998; 26:277-281. |
| Chang H. et al., Development of a topical suspension containing three active ingredient, Drug Dev and Ind Pharm, 28(1), 29-39 (2002). |
| Charles J. et al., 67Use of Bioerodible Polymers Impregnated with Mitomycin in Glaucoma Filtration Surgery in Rabbits, Ophthalmology, Apr. 1991; 98(4): 503-508. |
| Chen et al., Lumigan®: A Novel Drug for Glaucoma Therapy, Optometry in Practice, 2002; 3:95-102. |
| Cheng, Cheng-Kuo et al., Intravitreal Sustained-Release Dexamethasone Device in the Treatment of Experimental Uveitis, Investigative Ophthalmology & Visual Science, Feb. 1995, vol. 36, No. 2, pp. 442-453. |
| Chiang et al., Pharmacokinetics and Intraocular Pressure Lowering Effect of Timolol Preparation in Rabbit Eyes, Journal of Ocular Pharmacology and Therapeutics, 1996; 12(4):471-480. |
| Clark, D. Dick et al, The Influence of Triamcinolone Acetonide on Joint Stiffness in the Rat, The Journal of Bone and Joint Surgery, 1971, 1409-1414, 53A (7). |
| Cohen, Miriam et al, Organization and Adhesive Properties of the Hyaluronan Pericellular Coat of Chondrocytes and Epithelial Cells, Biophysical Journal, Sep. 2003, 1996-2005, 85. |
| Coleman et al., A 3-Month Randomized Controlled Trial of Bimatoprost (LUMIGAN) Versus Combined Timolol and Dorzolamide (Cosopt) in Patients with Glaucoma or Ocular Hypertension, Ophthalmology, 2003; 110(12):2362-2368. |
| Company News on Call, "Oculex Announces Positive Clinical Results for Posurdex(R)-The First Biodegradable Ocular Implant in Clinical Trial" Copyright © 1996-2004 PR Newswire Association LLC. |
| Coquelet et al., Successful Photodynamic Therapy Combined with Laser Photocoagulation in Three Eyes with Classic Subfoveal Choroidal Neovascularization Affecting Two Patients with Multifocal Choroiditis: Case Reports, Bulletin of the Society of Belgian Ophthalmologists, 2002; 283:69-73. |
| Crabb et al., Cloning of the cDNAs encoding the cellular retinaldehyde-binding protein from bovine and human retina and comparison of the protein structures, Journal of Biological Chemistry, 1988; 263(35):18688-18692. |
| Danis R. et al., Intravitreal triamcinolone acetonide in exudative age-related macular degeneration, Retina 2000; 20:244-250. |
| Dea I. et al., Hyaluronic acid: a novel, double helical molecule, Science, Feb. 9, 1973;179(73):560-2. |
| Deland, Frank, Intrathecal Toxicity Studies with Benzyl Alcohol, Toxicology and Applied Pharmacology, 1973, 153-6, 25, Academic Press, Inc. |
| Di Colo G., Controlled Drug Release From Implantable Matrices Based On Hydrophobic Polymers, Biomaterials, 1992; 13(12):850-856. |
| Dunn et al., ARPE-19, a human retinal pigment epithelial cell line with differentiated properties, Experimental Eye Research, 1996; 62:155-169. |
| Edelman et al., Corticosteroids inhibit VEGF-induced vascular leakage in a rabbit model of blood-retinal and blood-aqueous barrier breakdown, Exp Eye Res Feb. 2005;80(2):249-58. |
| Einmahl S. et al, Evaluation of a novel biomaterial in the suprachoroidal space of the rabbit eye, Invest Ophthal & Vis Sci 43(5); 1533-1539 (2002). |
| Einmahl S. et al, Therapeutic applications of viscous and injectable poly(ortho esters), Adv Drug Del Rev 53 (2001) 45-73. |
| Enyedi, Laura et al., An Intravitreal Device Providing Sustained Release of Cyclosporine and Dexamethason, Current Eye Research (1995) pp. 549-557. |
| Epstein, David L., Primary Open-Angle Glaucoma, Chandler and Grant's Glaucoma, Lea & Febiger, 1986; 129-181. |
| Fabbro et al., Protein tyrosine kinase inhibitors: new treatment modalitites?, Current Opinion in Pharmacology, 2002; 2:374-381. |
| Fokjaet et al, "Pharmaceutical Formulation Development of Peptides and Proteins", Taylor & Francis Limited, 2000, p. 131. |
| Fotsis et al., The endogenous oestrogen metabolite 2-methoxyoestradiol inhibits angiogenesis and suppresses tumor growth, Nature, 1994; 368:237. |
| Gaffney et al (Intra-articular triamcinolone hexacetonide in knee osteoarthritis: factors influencing the clinical response. Ann Rheum Dis. May 1995;54(5):379-81). |
| Geroski, Dayle et al, Drug Delivery for Posterior Segment Eye Disease, Investigative Ophthalmology & Visual Science, Apr. 2000, 961-964, 41(5). |
| Gilman, A.G. et al. eds., Goodman and Gilman's: The Pharmacological Basis of Therapeutics. 8th Edition, Pergamon Press: New York, 1990; 1447-1451. |
| Goel et al., Tyrosine Kinase Inhibitors: A Clinical Perspective, Current Oncology Reports, 2002; 4:9-19. |
| Goldberg V. et al., Hyaluronans in the treatment of osteoarthritis of the knee: evidence for disease-modifying activity, Osteoarthritis & Cartilage 2005; 13: 216-224. |
| Grecomoro, G. et al, Intra-articular treatment with sodium hyaluronate in gonarthrosis: a controlled clinical trial versus placebo, Pharmatherapeutica, 1987, 137-141, 5 (2). |
| Guenther, Lyn C., Optimizing Treatment with Topical Tazarotene, American Journal of Clinical Dermatology, 2003; 4(3):197-202. |
| Hainsworth, Dean P. et al., Sustained Release Intravitreal Dexamethasone, Journal of Ocular Pharmacology and Therapeutics, (1996) vol. 12, No. 1, pp. 57-63. |
| Haluska et al., Receptor tyrosine kinase inhibitors, Current Opinion in Investigational Drugs, 2001; 2(2):280-286. |
| Hamel et al., Molecular cloning and expression of RPE65, a novel retinal pigment epithelium-specific microsomal protein that is post-transcriptionally regulated in vitro, Journal of Biological Chemistry, 1993; 268(21):15751-15757. |
| Hare et al., Efficacy and safety of memantine, an NMDA-Type Open-Channel Blocker, for reduction of retinal injury associated with experimental glaucoma in rat and monkey, Survey of Ophthalmology, 2001; 45(Suppl 3):S284-S289. |
| Hashizoe, Mototane et al., Scleral Plug of Biodegradable Polymers for Controlled Drug Release in the Vitreous, Archives of Ophthalmology, 1994; 112:1380-1384. |
| Heller J., Biodegradable Polymers in Controlled Drug Delivery, CRC Critical Reviews in Therapeutic Drug Carrier Systems, 1987; 1(1):39-90 |
| Heller J., Hydrogels in Medicine and Pharmacy, N.A. Peppes ed., CRC Press, Boca Raton, FL, 1987; 3:137-149. |
| Helliwell P., Use of an objective measure of articular stiffness to record changes in finger joints after intra-articular injection of corticosteroid, Ann Rheum Dis 1997;56:71-73. |
| Hertzberger-ten Cate R. et ai., Intra-articular steroids in pauciarticular juvenile chronic arthritis, type I, Eur J Ped 1991 150: 170-172. |
| Hetherington, N.J. and M.J. Dooley, Potential for patient harm from intrathecal administration of preserved solutions. Med J Aust, 2000. 173(3): p. 141. |
| Hoyng et al., Pharmacological Therapy for Glaucoma, Drugs, Mar. 2000; 59(3):411-434. |
| Hubbard et al., Protein tyrosine kinase structure and function, Annual Review of Biochemistry, 2000; 69:373-398. |
| Hurst, E.W., Adhesive Arachnoiditis and Vascular Blockage caused by Detergents and Other Chemical Irritants: an Experimental Study. J. Path. Bact., 1955. 70: p. 167. |
| Inoue M. et al., Vitreous concentrations of triamcinolone acetonide in human eyes after intravitreal or subtenon injection, Am J Opth 138(6); 1046-1048: 2004. |
| Ioftsson T. et ai., Determination of Aqueous Solubility by Heating and Equilibration: A Technical Note, AAPS PharmSciTech. 5 2006;7(1): Article 4.001:1 0.1208/pt0701 04. |
| Jackanicz et al., Polyactic Acid as a biodegradable carrier for contraceptive steroids, Contraception, 1973; 8(3):227-235. |
| Jampel H. et al, Glaucoma Filtration Surgery in Monkeys Using 5-Fluorouridine in Polyanhydride Disks, Archives of Ophthalmology, Mar. 1990; 108:430-435. |
| Jonas J. et al., Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema, Am J Ophthalmol 2001; 132:425-427. |
| Jonas J. et al., Intravitreal injection of crystalline cortisone as adjunctive treatment of proliferative vitreoretinopathy, Br J Ophthalmol 2000; 84:1064-1067. |
| Jonas J. et al., Intravitreal injection of triamcinolone for diffuse diabetic macular edema, Arch Ophthalmol 2003; 121:57-61. |
| Jones, Adrian et al, Intra-articular Hyaluronic Acid Compared to Intra-articular Triamcinolone Hexacetonide in Inflammatory Knee Osteoarthritis, Osteoarthritis and Cartilage, 1995, 269-273, 3. |
| Kimura, Hideya et al., A New Vitreal Drug Delivery System using an Implantable Biodegradable Polymeric Device, Investigative Ophthalmology & Visual Science, 1994; 35:2815-2819. |
| Klimanskaya et al., Derivation and comparative assessment of retinal pigment epithelium from human embryonic stem cells using transcriptomics, Cloning and Stem Cells, 2004; 6(3):217-245. |
| Kochinke, F. et al., Biodegradable Drug Delivery System for Uveitis Treatment, Investigative Ophthalmology & Visual Science, Feb. 15, 1996, vol. 37. No. 3, 186-B98. |
| Kompella et al., Subconjunctival Nano- and Microparticles Sustain Retinal Delivery of Budesonide, a Corticosteroid Capable of Inhibiting VEGF Expression, Investigative Ophthalmology and Visual Science, Mar. 2003; 44(3):1192-1201. |
| Kopp, Sigvard et al, The Short-term Effect of Intra-articular Injections of Sodium Hyaluronate and Corticosteroid on Temporomandibular Joint Pain and Dysfunction, Journal of Oral and Maxillofacial Surgery, 1985, 429-435, 43. |
| Kwak, H.W. and D'Amico, D.J., Evaluation of the Retinal Toxicity and Pharmacokinetics of Dexamethasone After Intravitreal Injection, Archives of Ophthalmology, 1992; 110:259-266. |
| Lai et al., Alph-2 adrenoceptor agonist protects retinal function after acute retinal ischemic injury in the rat, Visual Neuroscience, 2002; 19:175-185. |
| Lee D. et al, The Use of Bioerodible Polymers and 5-Fluorouracil in Glaucoma Filtration Surgery, Investigative Ophthalmology & Visual Science, Nov. 1988; 29(11):1692-1697. |
| Lee D. et al., Glaucoma Filtration Surgery in Rabbits Using Bioerodible Polymers and 5-Fluorouracil, Ophthalmology, Dec. 1987; 94(12):1523-1530. |
| Liao, Y-H., et al., Hyaluronan: pharmaceutical characterization and drug delivery, Drug Delivery, 12: 327-342, 2005. |
| Mancinelli, Laviero et al, Intramuscular High-dose Triamcinolone Acetonide in the Treatment of Severe Chronic Asthma, West J Med, 1997, 322-329, 167 (5). |
| Marks R., Topical Tazarotene: Review and Re-Evaluation, Retinoids, 2001; 17(3):72-74. |
| Martidis A. et al., Intravitreal triamcinolone for refractory diabetic macular edema, Ophthalmology 2002; 109:920-927. |
| Maurice, D.M., Micropharmaceutics of the Eye, Ocular Inflammation Therapy, 1983; 1:97-102. |
| McCarty D., et al., Inflammatory reaction after intrasynovial injection of microcrystalline adrenocorticosteroid esters, Arthritis and Rheumatism, 7(4); 359-367 (1964). |
| McCarty, Daniel et al, Inflammatory Reaction after Intrasynovial Injection of Microcrystalline Adrenocorticosteroid Esters, Arthritis and Rheumatism, 1964, 359-367, 7 (4). |
| McCuen B. et al., The lack of toxicity of intravitreally administered triamcinolone acetonide, Am J Ophthalmol 1981; 91:785-788. |
| McGhee et al., Locally Administered Ocular Corticosteroids Benefits and Risks; Drug Safety, 2002; 25(1):33-55. |
| Miller et al., Degradation rates of oral resorbable implants (polyactates and polyglycolates) rate modification with changes in PLA/PGA copolymer ratios, Journal of Biomedical Materials Research, 1977; 11:711-719. |
| Miller et al., Synthesis and structure-activity profiles of A-Homoestranes, the Estratopones, Journal of Medical Chemistry, 1997; 40:3836-3841. |
| Morita Y., et al., Intravitreous delivery of dexamethasone sodium m-sulfobenzoate from poly (DL-lactic acid) implants, Biological and Pharmaceutical Bulletin, Feb. 1998; 21(2): 188-90. |
| Nauck M. et al., Corticosteroids inhibit the expression of the vascular endothelial growth factor gene in human vascular smooth muscle cells, Euro J Pharmacol 1998; 341:309-315. |
| Nauck M. et al., Induction of vascular endothelial growth factor by platelet-activating factor and platelet-derived growth factor is downregulated by corticosteroids, Am J Resp Cell Mol Biol 1997; 16:398-406. |
| Nauck, M., et al., Corticosteroids inhibit the expression of the vascular endothelial growth factor gene in human vascular smooth muscle cells, European Journal of Pharmacology, 1998; 341:309-315. |
| Nishimura A. et al., Isolating Triamcinolone acetonide particles for intravitreal use with a porous membrane filter, Retina, vol. 23(6); 777-779 (2003). |
| Olsen, T.W. et al., Human Scleral Permeability: Effects of Age, Cryotherapy, Transscleral Diode Laser, and Surgical Thinning, Investigative Ophthalmology & Visual Science, 1995; 36(9):1893-1903. |
| Pe'er J. et al., Vascular endothelial growth factor upregulation in human central retinal vein occlusion, Ophthalmology 1998; 105:412-416. |
| Penfold P. et al., Exudative macular degeneration and intravitreal triamcinolone: A pilot study, Aust NZ J Ophthalmol 1995; 23:293-298. |
| Phillips et al., Efficacy of 0.1% Tazarotene cream for the treatment of photodamage, Archives of Dermatology, Nov. 2002; 138(11):1486-1493. |
| Phillips et al., Penetration of timolol eye drops into human aqueous humour: the first hour, British Journal of Ophthalmology, 1985; 69:217-218. |
| Physician's Desk Reference for Ophthalmic Medicines, 30 Edition, 2002; 285. |
| Physician's Desk Reference, product information on "Alphagan®P", 54 Edition, 2000; 494-494. |
| Pinheiro M. et ai., Adverse effect of soft tissue augmentation with hyaluronic acid, J Cosmet Dermatol. 2005; 4: 184-6. |
| Pribluda et al., 2-Methoxyestradiol: an endogenous antiangiogenic and antiproliferative drug candidate, Cancer and Metastasis Reviews, 2000; 19:173-179. |
| Quigley et al., The mechanism of optic nerve damage in experimental acute intraocular pressure elevation, Investigative Ophthalmology & Visual Science, 1980; 19:505. |
| Rao et al., Preparation and Evaluation of Ocular Inserts Containing Norfloxacin, Turkish Journal of Medical Science, 2004; 34:239-246. |
| Rao, N.A. et al., Introcular Inflammation and Uveitis, In Basic and Clinical Science Course, San Francisco: American Academy of Ophthalmology, 1997-1998; section 9, 5780, 102-103, 152-156. |
| Rechtman et al., Intravitreal triaminolone with photodynamic therapy for subfoveal choroidal neovascularisation in age related macular degeneration, British Journal of Ophthalmology, 2004; 88:344-347. |
| Renfro, L. et al., Ocular Effects of Topical and Systemic Steroids, Dermatologic Clinics, 1992; 10:505-512. |
| Rogojina et al., Comparing the use of Affymetrix to spotted oligonucleotide microarrays using two retinal pigment epithelium cell lines, Molecular Vision, 2003; 9:482-496. |
| Roth D. et al., Noninfectious endophthalmitis associated with intravitreal triamcinolone injection, Arch Opthalmol 2003; 121: 1279-1282. |
| Schindler R. et al., The clearance of intravitreal triamcinolone acetonide, Am J Ophthalmol 1982; 93:415-417. |
| Scholes G. et al., Clearance of triamcinolone from vitreous, Arch Ophthalmol 1985; 103:1567-1569. |
| Schuettauf et al., Effects of anti-glaucoma medications on ganglion cell survival: the DBA/2J mouse model, Vision Research, 2002; 42(20):2333-2337. |
| Schumacher et al., The physiological estrogen metabolite 2-methoxyestradiol reduced tumor growth and induces apoptosis in human solid tumors, Journal of Cancer Research and Clinical Oncology, 2001; 127:405-410. |
| Schwartz, B., The Response of Ocular Pressure to Corticosteroids, Ophthalmology Clinics of North America; 1966; 6:929-989. |
| Selvi, Enrico et al, Arthritis Induced by Corticosteroid Crystals, The Journal of Rheumatology, 2004, 622, 31 (3). |
| Siebold et al., Prodrug 5, 3 (1989). |
| Skalka, H.W. et al., Effect of Corticosteroids on Cataract Formation, Archives of Ophthalmology, 1980; 98:1773-1777. |
| Smith et al., Sustained-release subconjunctival 5-fluorouracil, Ophthalmic Surgery and Laser, Sep. 1996; 27(9):763-767. |
| Starr, M.S., Further Studies on the Effect of Prostaglandin on Intraocular Pressure in the Rabbit, Experimental Eye Research, 1971; 11:170-177. |
| Streilein et al., Ocular immune privilege: therapeutic opportunities from an experiment of nature, Nature Reviews Immunology, 2003; 3:879-889. |
| Survey of Ophthalmology 2002; 47(3); 295. |
| Sutter F. et al., Pseudo-endophthalmitis after intravitreal injection of triamcinolone, Br J Ophthalmol 2003; 87:972-974. |
| Tan, D.T.H. et al., Randomized Clinical Trial of a New Dexamethasone Delivery System (Surodex) for Treating of Post-Cataract Surgery Inflammation, Ophthalmology, 1999; 106(2):223-231. |
| Tracy et al., Factors affecting the degradation rate of poly (lactide-co-glycolide) Microspheres in vivo and in vitro, Biomaterials, 1999; 20:1057-1062. |
| U.S. Appl. No. 60/567,339, filed Apr. 2004, Hughes. |
| U.S. Appl. No. 60/567,423, filed Apr. 2004, Hughes. |
| U.S. Appl. No. 60/587,092, filed Jul. 2004, Whitcup. |
| United States Pharmacopeia, The National Formulary; USP 23/NF 18; 1995; pp. 1790-1798. |
| Watson et al., A Six-month, Randomized, Double-masked Study Comparing Latanoprost with Timolol in Open-angle Glaucoma and Ocular Hypertension, Ophthalmology, 1996; 103:126-137. |
| Wheeler et al, Role of Alpha-2 Agonists in Neuroprotection, Survey of Ophthalmology, Apr. 2003; 48(Suppl 1):S47-S51. |
| Wheeler, Experimental studies of agents with potential neuroprotective properties, Acta Ophthalmologica Scandinavica, 1999; 77(229):27-28. |
| WoldeMussie et al., Neuroprotective effects of memantine in different retinal injury models in rats, Journal of Glaucoma, 2002; 11(6):474-480. |
| WoldeMussie, Neuroprotection of retinal ganglion cells in experimental models of glaucoma, Minerva Oftalmol, 2000; 42(2):71-78. |
| Woodward et al., "The Pharmacology of Bimatoprost (Lumigan™)", Survey of Ophthalmology, 2001; 45(Suppl 4): S337-S345. |
| Woodward et al., AGN 2024 (Lumigan®): A Synthetic Prostamide Analog that Lowers Primate Intraocular Pressure by Virtue of Its Inherent Pharmacological Activity, ARVO 2002; (CD-ROM):POS. |
| Yang J. et ai., Transdermal delivery system of triamcinolone acetonide from a gel using phonophoresis, Arch Pharm Res 29(5); 412-417: 2006. |
| Yeung et al., Cytotoxicity of Triamcinolone on Cultured Human Retinal Pigment Epithelial Cells: Comparison with Dexamethasone and Hydrocortisone, Japanese Journal of Ophthalmology, 2004; 48:236-242. |
| Zhou, T. et al., Development of a Multiple-Drug Delivery Implant for Introcular Management of Proliferative Vitreoretinopathy, Journal of Controlled Release, 1998; 55:281-295. |
| Zulian, F. et al, Triamcinolone Acetonide and Hexacetonide Intra-articular Treatment of Symmetrical Joints in Juvenile Idiopathic Arthritis: A Double-blind Trial, Rheumatology, 2004, 1288-1291, 43. |
Cited By (10)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20160038396A1 (en) * | 2007-12-12 | 2016-02-11 | Allergan, Inc. | Dermal filler |
| US9622957B2 (en) * | 2007-12-12 | 2017-04-18 | Allergan, Inc. | Dermal filler |
| US9833460B2 (en) | 2013-01-23 | 2017-12-05 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US10744144B2 (en) | 2013-01-23 | 2020-08-18 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US11364251B2 (en) | 2013-01-23 | 2022-06-21 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US12016867B2 (en) | 2013-01-23 | 2024-06-25 | Semnur Pharmaceuticals, Inc. | Methods of treating inflammation and/or pain |
| US10117938B2 (en) | 2015-01-21 | 2018-11-06 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US10500284B2 (en) | 2015-01-21 | 2019-12-10 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US11020485B2 (en) | 2015-01-21 | 2021-06-01 | Semnur Pharmaceuticals, Inc. | Pharmaceutical formulation |
| US12285485B2 (en) | 2015-01-21 | 2025-04-29 | Semnur Pharmaceuticals, Inc. | Methods of treating pain |
Also Published As
| Publication number | Publication date |
|---|---|
| US20080044476A1 (en) | 2008-02-21 |
| US20070224278A1 (en) | 2007-09-27 |
| US8846094B2 (en) | 2014-09-30 |
| US20140356438A1 (en) | 2014-12-04 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US9089478B2 (en) | Peripherally administered viscous formulations | |
| JP5592321B2 (en) | Compositions and methods for treatment of the back of the eye | |
| AU2009223649B2 (en) | Low viscosity, highly flocculated triamcinolone acetonide suspensions for intravitreal injection | |
| US20060141049A1 (en) | Triamcinolone compositions for intravitreal administration to treat ocular conditions | |
| TWI674899B (en) | Pharmaceutical formulation | |
| CN1852700A (en) | Triamcinolone acetonide and anecortave acetate formulations for injection | |
| US20090149435A1 (en) | Process for making a pharmaceutical composition | |
| US20250120985A1 (en) | Method of treating diabetic macular edema | |
| ZA200603549B (en) | Compositions and methods for treating a posterior segment of an eye | |
| WO2025169089A1 (en) | Ophthalmic compositions of tyrosine kinase inhibitors and their uses | |
| RU2336074C2 (en) | Compositions and methods of treatment of posterior ocular segment | |
| MXPA06005146A (en) | Compositions and methods for treating a posterior segment of an eye |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| AS | Assignment |
Owner name: ALLERGAN, INC., CALIFORNIA Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNORS:LYONS, ROBERT T.;ROBINSON, MICHAEL R.;TROGDEN, JOHN T.;AND OTHERS;REEL/FRAME:033566/0249 Effective date: 20070725 |
|
| STCF | Information on status: patent grant |
Free format text: PATENTED CASE |
|
| MAFP | Maintenance fee payment |
Free format text: PAYMENT OF MAINTENANCE FEE, 4TH YEAR, LARGE ENTITY (ORIGINAL EVENT CODE: M1551); ENTITY STATUS OF PATENT OWNER: LARGE ENTITY Year of fee payment: 4 |
|
| MAFP | Maintenance fee payment |
Free format text: PAYMENT OF MAINTENANCE FEE, 8TH YEAR, LARGE ENTITY (ORIGINAL EVENT CODE: M1552); ENTITY STATUS OF PATENT OWNER: LARGE ENTITY Year of fee payment: 8 |