Dysphagia is difficulty in swallowing.[1][2] Although classified under "symptoms and signs" in ICD-10,[3] in some contexts it is classified as a condition in its own right.[4][5][6]
| Dysphagia | |
|---|---|
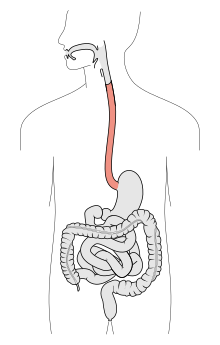 | |
| The digestive tract, with the esophagus marked in red | |
| Specialty | Gastroenterology, phoniatrics |
| Symptoms | Inability or difficulty swallowing |
| Complications | Pulmonary aspiration, malnutrition, starvation |
| Causes | Esophageal cancer, Esophagitis, Stomach cancer, mental illness, alcoholism, refeeding syndrome, starvation, infection, gastritis, malnutrition |
It may be a sensation that suggests difficulty in the passage of solids or liquids from the mouth to the stomach,[7] a lack of pharyngeal sensation or various other inadequacies of the swallowing mechanism. Dysphagia is distinguished from other symptoms including odynophagia, which is defined as painful swallowing,[8] and globus, which is the sensation of a lump in the throat. A person can have dysphagia without odynophagia (dysfunction without pain), odynophagia without dysphagia (pain without dysfunction) or both together. A psychogenic dysphagia is known as phagophobia.[9]
Classification
editDysphagia is classified into the following major types:[10]
- Oropharyngeal dysphagia
- Esophageal and obstructive dysphagia
- Neuromuscular symptom complexes
- Functional dysphagia is defined in some patients as having no organic cause for dysphagia that can be found.
Signs and symptoms
editSome patients have limited awareness of their dysphagia, so lack of the symptom does not exclude an underlying disease.[11] When dysphagia goes undiagnosed or untreated, patients are at a high risk of pulmonary aspiration and subsequent aspiration pneumonia secondary to food or liquids going the wrong way into the lungs. Some people present with "silent aspiration" and do not cough or show outward signs of aspiration. Undiagnosed dysphagia can also result in dehydration, malnutrition, and kidney failure.[12]
Some signs and symptoms of oropharyngeal dysphagia include difficulty controlling food in the mouth, inability to control food or saliva in the mouth, difficulty initiating a swallow, coughing, choking, frequent pneumonia, unexplained weight loss, gurgly or wet voice after swallowing, nasal regurgitation, and patient complaint of swallowing difficulty.[11] When asked where the food is getting stuck, patients will often point to the cervical (neck) region as the site of the obstruction. The actual site of obstruction is always at or below the level at which the level of obstruction is perceived.[citation needed]
The most common symptom of esophageal dysphagia is the inability to swallow solid food, which the patient will describe as 'becoming stuck' or 'held up' before it either passes into the stomach or is regurgitated. Pain on swallowing or odynophagia is a distinctive symptom that can be highly indicative of carcinoma, although it also has numerous other causes that are not related to cancer. Achalasia is a major exception to usual pattern of dysphagia in that swallowing of fluid tends to cause more difficulty than swallowing solids. In achalasia, there is idiopathic destruction of parasympathetic ganglia of the Auerbach's (Myenteric) plexus of the entire esophagus, which results in functional narrowing of the lower esophagus, and peristaltic failure throughout its length.[13]
Complications
editComplications of dysphagia may include aspiration, pneumonia, dehydration, and weight loss.[14]
Causes
editThe following table enumerates possible causes of dysphagia:
| Location | Cause |
|---|---|
| Oral dysphagia |
|
| Pharyngeal dysphagia |
|
| Esophageal dysphagia |
|
Difficulty with or inability to swallow may be caused or exacerbated by usage of opiate and/or opioid drugs.[15]
Diagnosis
edit- Esophagoscopy and laryngoscopy can give direct view of lumens.
- Esophageal motility study is useful in cases of esophageal achalasia and diffuse esophageal spasms.
- Exfoliative cytology can be performed on esophageal lavage obtained by esophagoscopy. It can detect malignant cells in early stage.
- Ultrasonography and CT scan are not very useful in finding causes of dysphagia, but can detect masses in mediastinum and aortic aneurysms.
- FEES (Fibreoptic endoscopic evaluation of swallowing), sometimes with sensory evaluation, is done usually by a Medical Speech Pathologist or Deglutologist. This procedure involves the patient eating different consistencies as above.
- Swallowing sounds and vibrations could be potentially used for dysphagia screening, but these approaches are in the early research stages.[16]
Differential diagnosis
editAll causes of dysphagia are considered as differential diagnoses. Some common ones are:[17]
- Esophageal atresia
- Paterson-Kelly syndrome
- Zenker's diverticulum
- Esophageal varices
- Benign strictures
- Achalasia
- Esophageal diverticula
- Scleroderma[18]
- Diffuse esophageal spasm
- Polymyositis
- Webs and rings
- Esophageal cancer[19]
- Eosinophilic esophagitis[20]
- Hiatus hernia, especially paraesophageal type
- Dysphagia lusoria
- Stroke
- Fahr's disease
- Wernicke encephalopathy
- Charcot–Marie–Tooth disease
- Parkinson's disease
- Multiple sclerosis
- Amyotrophic lateral sclerosis
- Rabies
- Cervical Spondylosis[21]
Esophageal dysphagia is almost always caused by disease in or adjacent to the esophagus but occasionally the lesion is in the pharynx or stomach. In many of the pathological conditions causing dysphagia, the lumen becomes progressively narrowed and indistensible. Initially, only fibrous solids cause difficulty but later the problem can extend to all solids and later even to liquids. Patients with difficulty swallowing may benefit from thickened fluids if the person is more comfortable with those liquids, although, so far, there is no scientific study that proves that those thickened liquids are beneficial.[22]
Dysphagia may manifest as the result of autonomic nervous system pathologies including stroke[23] and ALS,[24] or due to rapid iatrogenic correction of an electrolyte imbalance.[25]
In older adults, presbyphagia - the normal healthy changes in swallowing associated with age - should be considered as an alternative explanation for symptoms.[26]
Treatments
editThere are many ways to treat dysphagia, such as swallowing therapy, dietary changes, feeding tubes, certain medications, and surgery. Treatment for dysphagia is managed by a group of specialists known as a multidisciplinary team. Members of the multidisciplinary team include: a speech language pathologist specializing in swallowing disorders (swallowing therapist), primary physician, gastroenterologist, nursing staff, respiratory therapist, dietitian, occupational therapist, physical therapist, pharmacist, and radiologist.[11] The role of the members of the multidisciplinary team will differ depending on the type of swallowing disorder present. For example, the swallowing therapist will be directly involved in the treatment of a patient with oropharyngeal dysphagia, while a gastroenterologist will be directly involved in the treatment of an esophageal disorder.[citation needed]
Treatment strategies
editThe implementation of a treatment strategy should be based on a thorough evaluation by the multidisciplinary team. Treatment strategies will differ on a patient to patient basis and should be structured to meet the specific needs of each individual patient. Treatment strategies are chosen based on a number of different factors including diagnosis, prognosis, reaction to compensatory strategies, severity of dysphagia, cognitive status, respiratory function, caregiver support, and patient motivation and interest.[11]
Oral vs. nonoral feeding
editAdequate nutrition and hydration must be preserved at all times during dysphagia treatment. The overall goal of dysphagia therapy is to maintain or return the patient to, oral feeding. However, this must be done while ensuring adequate nutrition and hydration and a safe swallow (no aspiration of food into the lungs).[11] If oral feeding results in increased mealtimes and increased effort during the swallow, resulting in not enough food being ingested to maintain weight, a supplementary nonoral feeding method of nutrition may be needed. In addition, if the patient aspirates food or liquid into the lungs despite the use of compensatory strategies, and is therefore unsafe for oral feeding, nonoral feeding may be needed. Nonoral feeding includes receiving nutrition through a method that bypasses the oropharyngeal swallowing mechanism including a nasogastric tube, gastrostomy, or jejunostomy.[11] Some people with dysphagia, especially those nearing the end of life, may choose to continue eating and drinking orally even when it has been deemed unsafe. This is known as "risk feeding".[27]
Swallowing difficulties in dementia
editA 2018 Cochrane review found no certain evidence about the immediate and long-term effects of modifying the thickness of fluids for swallowing difficulties in people with dementia.[28] While thickening fluids may have an immediate positive effect on swallowing and improving oral intake, the long-term impact on the health of the person with dementia should also be considered.[22]
Treatment procedures
editCompensatory treatment procedures are designed to change the flow of the food/liquids and eliminate symptoms but do not directly change the physiology of the swallow.[11]
- Postural techniques
- Food consistency (diet) changes
- Modifying volume and speed of food presentation
- Technique to improve oral sensory awareness
- Intraoral prosthetics
Therapeutic treatment procedures – designed to change and/or improve the physiology of the swallow.[11][29]
- Oral and pharyngeal range-of-Motion exercises
- Resistance exercises
- Bolus control exercises
- Swallowing maneuvers
- Supraglottic swallow
- Super-supraglottic swallow
- Effortful swallow
- Mendelsohn maneuver
Patients may need a combination of treatment procedures to maintain a safe and nutritionally adequate swallow. For example, postural strategies may be combined with swallowing maneuvers to allow the patient to swallow in a safe and efficient manner.[citation needed]
The most common interventions used for those with oropharyngeal dysphagia by speech language pathologists are rehabilitation of the swallow through oral motor exercises, texture modification of foods, thickening fluids and positioning changes during swallowing.[30] The effectiveness of modifying food and fluid in preventing aspiration pneumonia has been questioned and these can be associated with poorer nutrition, hydration and quality of life.[31] Also, there has been considerable variability in national approaches to describing different degrees of thickened fluids and food textures. However, in 2015, the International Dysphagia Diet Standardisation Initiative (IDDSI) group produced an agreed IDDSI framework consisting of a continuum of 8 levels (0–7), where drinks are measured from Levels 0 – 4, while foods are measured from Levels 3 – 7.[32] It is likely that this initiative, which has widespread support among dysphagia practitioners, will improve communication with carers and will lead to greater standardisation of modified diets[citation needed]
Epidemiology
editSwallowing disorders can occur in all age groups, resulting from congenital abnormalities, structural damage, and/or medical conditions.[11] Swallowing problems are a common complaint among older individuals, and the incidence of dysphagia is higher in the elderly,[33][34] and in patients who have had strokes.[35] Dysphagia affects about 3% of the population.[36]
Etymology
editThe word "dysphagia" is derived from the Greek dys meaning bad or disordered, and the root phag- meaning "eat".[citation needed]
See also
edit- Aphagia
- MEGF10
- Pseudodysphagia, an irrational fear of swallowing or choking
References
edit- ^ Smithard DG, Smeeton NC, Wolfe CD (January 2007). "Long-term outcome after stroke: does dysphagia matter?". Age and Ageing. 36 (1): 90–94. doi:10.1093/ageing/afl149. PMID 17172601.
- ^ Brady A (January 2008). "Managing the patient with dysphagia". Home Healthcare Nurse. 26 (1): 41–46, quiz 47–48. doi:10.1097/01.NHH.0000305554.40220.6d. PMID 18158492. S2CID 11420756.
- ^ "ICD-10". Retrieved 23 February 2008.
- ^ Boczko F (November 2006). "Patients' awareness of symptoms of dysphagia". Journal of the American Medical Directors Association. 7 (9): 587–90. doi:10.1016/j.jamda.2006.08.002. PMID 17095424.
- ^ "Dysphagia". University of Virginia. Archived from the original on 9 July 2004. Retrieved 24 February 2008.
- ^ "Swallowing Disorders – Symptoms of Dysphagia". New York University School of Medicine. Archived from the original on 14 November 2007. Retrieved 24 February 2008.
- ^ Sleisenger MH, Feldman M, Friedman LM (2002). Sleisenger & Fordtran's Gastrointestinal & Liver Disease, 7th edition. Philadelphia, PA: W.B. Saunders Company. pp. Chapter 6, p. 63. ISBN 978-0-7216-0010-9.
- ^ "Dysphagia". University of Texas Medical Branch. Archived from the original on 6 March 2008. Retrieved 23 February 2008.
- ^ Franko, Debra L.; Shapiro, Jo; Gagne, Adele (1997). "Phagophobia: A form of Psychogenic Dysphagia a New Entity". Annals of Otology, Rhinology & Laryngology. 106 (4). SAGE Publications: 286–290. doi:10.1177/000348949710600404. ISSN 0003-4894. PMID 9109717. S2CID 22215557.
- ^ Spieker MR (June 2000). "Evaluating dysphagia". American Family Physician. 61 (12): 3639–48. PMID 10892635.
- ^ a b c d e f g h i Logemann, Jeri A. (1998). Evaluation and treatment of swallowing disorders. Austin, Tex: Pro-Ed. ISBN 978-0-89079-728-0.
- ^ Reber; Gomes; Dähn; Vasiloglou; Stanga (8 November 2019). "Management of Dehydration in Patients Suffering Swallowing Difficulties". Journal of Clinical Medicine. 8 (11). MDPI AG: 1923. doi:10.3390/jcm8111923. ISSN 2077-0383. PMC 6912295. PMID 31717441.
- ^ "Achalasia". The Lecturio Medical Concept Library. 14 October 2020. Retrieved 12 July 2021.
- ^ Rofes, Laia; Arreola, Viridiana; Almirall, Jordi; Cabré, Mateu; Campins, Lluís; García-Peris, Pilar; Speyer, Renée; Clavé, Pere (2011). "Diagnosis and Management of Oropharyngeal Dysphagia and Its Nutritional and Respiratory Complications in the Elderly". Gastroenterology Research and Practice. 2011. Hindawi Limited: 1–13. doi:10.1155/2011/818979. ISSN 1687-6121. PMC 2929516. PMID 20811545.
- ^ Savilampi, Johanna (31 January 2012). "Opioid Effects on Swallowing and Esophageal Sphincter Pressure". clinicaltrials.gov. US National Library of Medicine. Retrieved 23 March 2018.
- ^ Dudik JM, Coyle JL, Sejdić E (August 2015). "Dysphagia Screening: Contributions of Cervical Auscultation Signals and Modern Signal-Processing Techniques". IEEE Transactions on Human-Machine Systems. 45 (4): 465–477. doi:10.1109/thms.2015.2408615. PMC 4511276. PMID 26213659.
- ^ "Dysphagia". The Lecturio Medical Concept Library. Retrieved 12 July 2021.
- ^ "Scleroderma". The Lecturio Medical Concept Library. Retrieved 22 July 2021.
- ^ "Esophageal Cancer". The Lecturio Medical Concept Library. 26 October 2020. Retrieved 22 July 2021.
- ^ "Esophagitis". The Lecturio Medical Concept Library. Retrieved 22 July 2021.
- ^ Chu EC, Shum JS, Lin AF (2019). "Unusual Cause of Dysphagia in a Patient With Cervical Spondylosis". Clinical Medicine Insights: Case Reports. 12: 1179547619882707. doi:10.1177/1179547619882707. PMC 6937524. PMID 31908560.
- ^ a b Steele, Simon J.; Ennis, Samantha L.; Dobler, Claudia C. (2021). "Treatment burden associated with the intake of thickened fluids". Breathe. 17 (1). European Respiratory Society (ERS): 210003. doi:10.1183/20734735.0003-2021. ISSN 1810-6838. PMC 8291955. PMID 34295407.
- ^ Edmiaston J, Connor LT, Loehr L, Nassief A (July 2010). "Validation of a dysphagia screening tool in acute stroke patients". American Journal of Critical Care. 19 (4): 357–64. doi:10.4037/ajcc2009961. PMC 2896456. PMID 19875722.
- ^ Noh EJ, Park MI, Park SJ, Moon W, Jung HJ (July 2010). "A case of amyotrophic lateral sclerosis presented as oropharyngeal Dysphagia". Journal of Neurogastroenterology and Motility. 16 (3): 319–22. doi:10.5056/jnm.2010.16.3.319. PMC 2912126. PMID 20680172.
- ^ Martin RJ (September 2004). "Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes". Journal of Neurology, Neurosurgery, and Psychiatry. 75 (Suppl 3): iii22–28. doi:10.1136/jnnp.2004.045906. PMC 1765665. PMID 15316041.
- ^ "Resources: Presbyphagia/ or swallowing and ageing". Melbourne Swallow Analysis Centre. Retrieved 7 March 2022.
- ^ Supporting people who have eating and drinking difficulties. A guide to practical care and clinical assistance, particularly towards the end of life (2 ed.). London: Royal College of Physicians. 2021. ISBN 978-1-86016-796-6.
- ^ Flynn, Eadaoin; Smith, Christina H; Walsh, Cathal D; Walshe, Margaret (24 September 2018). "Modifying the consistency of food and fluids for swallowing difficulties in dementia". Cochrane Database of Systematic Reviews. 2018 (9): CD011077. doi:10.1002/14651858.cd011077.pub2. ISSN 1465-1858. PMC 6513397. PMID 30251253.
- ^ Perry A, Lee SH, Cotton S, Kennedy C, et al. (Cochrane ENT Group) (August 2016). "Therapeutic exercises for affecting post-treatment swallowing in people treated for advanced-stage head and neck cancers". The Cochrane Database of Systematic Reviews. 2016 (8): CD011112. doi:10.1002/14651858.CD011112.pub2. hdl:10059/1671. PMC 7104309. PMID 27562477.
- ^ McCurtin A, Healy C (February 2017). "Why do clinicians choose the therapies and techniques they do? Exploring clinical decision-making via treatment selections in dysphagia practice". International Journal of Speech-Language Pathology. 19 (1): 69–76. doi:10.3109/17549507.2016.1159333. PMID 27063701. S2CID 31193444.
- ^ O'Keeffe ST (July 2018). "Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified?". BMC Geriatrics. 18 (1): 167. doi:10.1186/s12877-018-0839-7. PMC 6053717. PMID 30029632.
- ^ Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, Duivestein J, Kayashita J, Lecko C, Murray J, Pillay M, Riquelme L, Stanschus S (April 2017). "Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework". Dysphagia. 32 (2): 293–314. doi:10.1007/s00455-016-9758-y. PMC 5380696. PMID 27913916.
- ^ Shamburek RD, Farrar JT (February 1990). "Disorders of the digestive system in the elderly". The New England Journal of Medicine. 322 (7): 438–43. doi:10.1056/NEJM199002153220705. PMID 2405269.
- ^ Span P (21 April 2010). "When the Meal Won't Go Down". The New York Times. Retrieved 27 July 2014.
- ^ Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R (December 2005). "Dysphagia after stroke: incidence, diagnosis, and pulmonary complications". Stroke. 36 (12): 2756–63. doi:10.1161/01.STR.0000190056.76543.eb. PMID 16269630.
- ^ Kim JP, Kahrilas PJ (January 2019). "How I Approach Dysphagia". Curr Gastroenterol Rep. 21 (10): 49. doi:10.1007/s11894-019-0718-1. PMID 31432250. S2CID 201064709.