INTRODUCTION
Spiders, especially brown recluses (Loxosceles reclusa) (figure 1), are frequently incriminated as causative agents in idiopathic wounds, even though diagnoses are usually made solely on the basis of dermatologic symptoms. Rarely is a spider seen inflicting the wound or captured while biting, and it is difficult to either prove or disprove spider participation in the event. The biologic distribution of the brown recluse and related recluse species indicates that many diagnoses made on cases occurring in the western United States are incorrect.1
Figure 1.
Dorsal view of the brown recluse spider, Loxosceles reclusa. The most consistent diagnostic feature for identification is the pattern of 6 eyes, grouped in pairs, with 1 anterior pair and 2 lateral pairs (most spiders have 8 eyes in 2 rows of 4). Although the violin pattern on the cephalothorax (body part to which legs attach) is commonly mentioned as a diagnostic characteristic, this feature can be indistinct or absent in immatures or in related recluse species. In addition, the abdomen is always monochromatic but can vary from tan to dark brown.
SOURCES OF INFORMATION
Because of my research interests in spider identification and medically important spiders, I have been avidly studying recluse spiders and their occurrence in the western United States. My experience is greatest in California, but the information presented here is pertinent to northern and western states as well. In almost a decade of research, I have found verification of fewer than 10 brown recluse specimens in California in more than 40 years of records. Sources include medical and arachnologic literature and correspondence with scores of arachnologists, county entomologists, vector control personnel, and the California Department of Food and Agriculture, which handles all exotic pest identifications in the state. Most verified specimens were individuals intercepted from facilities receiving goods from out of state. There are no populations of brown recluses in California.
MISDIAGNOSIS OF IDIOPATHIC WOUNDS
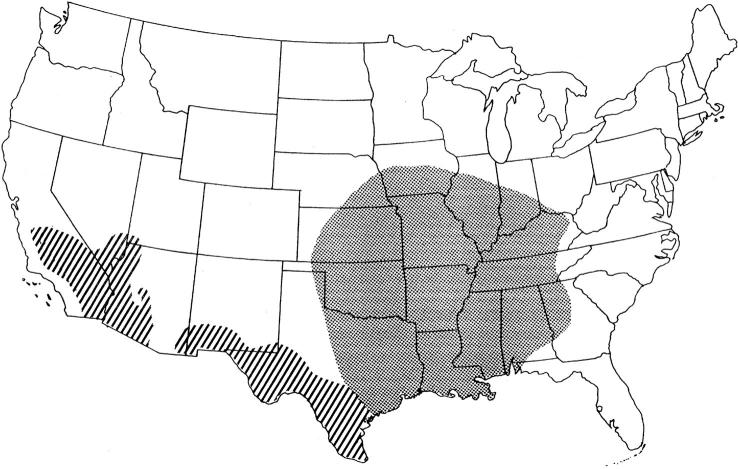
Despite the lack of brown recluse spiders in California, several hundred cases of “brown recluse bites” have been reported to me in the past decade. Undoubtedly, this is only a small fraction of the total number of brown recluse bites that have been diagnosed. Although it might appear intuitive from figure 2 that these bites could be caused by the native desert recluse (Loxosceles deserta), which lives in the comparatively sparsely inhabited southeastern quadrant of California, virtually all so-called brown recluse bites have come from coastal regions with a concentrated human population. In particular, many originate from the San Francisco Bay-Sacramento area, which lies north of the native desert recluse distribution (figure 2) and has never supported a population of any recluse species. Similar scenarios have emerged from other states, cities, or regions—Vermont, New York, Pennsylvania, Florida, Chicago, South Dakota, Colorado, northern Nevada—where recluse spiders are extremely rare (<10 ever collected) or have never been documented.2 There are published California accounts of 2 “brown recluse bite” case histories from a city where recluses have never been collected3 and a physician misidentification of a common spider as a brown recluse, captured while biting a child.4 Brown recluse bites are overdiagnosed in coastal and Northern California.
Figure 2.
Endemic distributions of the brown recluse (stippling) and related recluse species (lines) in the United States, based on Gertsch and Ennik.2 Recluse populations become sporadic on either side of the demarcating range borders.
CONDITIONS THAT CAN CAUSE NECROTIC WOUNDS AND/OR THAT HAVE BEEN MISDIAGNOSED AS BROWN RECLUSE BITES
Many conditions can cause necrotic wounds that have been misdiagnosed as brown recluse bites.5,6,7 Many of these are disease states in which an arthropod was not involved (box).
If arthropods are in fact implicated, physicians should not immediately think of accidental spider bites as the likely cause. Instead, they should consider creatures that seek mammals for blood meals—such as ticks, fleas, bedbugs, and assassin bugs—and whose bites can cause a variety of reactions.5,6
Tickborne Lyme disease can cause a “bull's-eye wound,” which is a diagnostic symptom of brown recluse envenomation, and so Lyme disease can be misdiagnosed as a brown recluse bite.8 Although Lyme disease occurs at low incidence in California,9 because it can lead to irreversible neural and cardiac complications, its misdiagnosis as a brown recluse bite could have grave consequences.
OTHER DIAGNOSES MAY COEXIST WITH SPIDER BITES
Even in cases of verified spider bite, differentiation must be made between toxic effects of venom and secondary infections, such as incurred when pruritus leads to scratching. Furthermore, rigorous clinical investigation might reveal alternative causative agents. For example, in 1 case report, a large spider bit an Australian woman, and therapy for the spider bite was ineffective. Subsequent screening determined that the “necrotic arachnidism” was actually a fungal infection called sporotrichosis,10 another condition misdiagnosed in the United States as brown recluse bite.5
OTHER SPIDERS IMPLICATED IN WOUNDS
Since the early 1980s, a European native, the hobo spider (Tegenaria agrestis), has been implicated in necrotic lesions.11 Although it lives in the Pacific Northwest, east to Montana and south into northern Utah, hobo spider bite diagnoses have already been made in California, even though it has never been documented in the state. The bite of the yellow sac spider (Cheiracanthium mildei), another European native, is usually minor but can cause mild necrosis.12 It was uncommon in the United States before 1950 but has since spread coast to coast, and it is often found in homes.
CONCLUSION
Physicians in nonendemic brown recluse regions (figure 2) should be cautious in implicating brown recluses in idiopathic necrotic wounds. The medical community needs to be aware of the many causes of necrotic wounds that can be misdiagnosed as recluse bites. Culture of specimens taken from wounds might accurately determine the plethora of causative agents of so-called brown recluse bites, which can vary from being arthropod, bacterial, viral, or fungal in nature or due to underlying disease states.
Conditions that can cause necrotic wounds and/or that have been misdiagnosed as brown recluse bites
Infections with Staphylococcus or Streptococcus species
Herpes simplex
Herpes zoster
Erythema multiforme
Diabetic ulcer
Lyme disease
Fungal infection
Pyoderma gangrenosum
Lymphomatoid papulosis
Chemical burn
Poison ivy/oak dermatitis
Squamous cell carcinoma
Localized vasculitis
Syphilitic chancre
Competing interests: None declared
Author: Rick Vetter is an entomologist at the University of California, Riverside. His medical arachnology research involves venomous spiders, misdiagnoses of their bites, and arachnophobia.
References
- 1.Vetter RS. Brown recluse and other recluse spiders: integrated pest management in and around the home. Univ Calif Pest Notes 2000;7468:1-4. Available at http://www.ipm.ucdavis.edu/PMG/PESTNOTES/pn7468.html.
- 2.Gertsch WJ, Ennik F. The spider genus Loxosceles in North America, Central America, and the West Indies (Araneae, Loxoscelidae). Bull Am Museum Natural Hist 1983;175: 264-360. [Google Scholar]
- 3.Salm RJ, Fee MJ, Giacopelli JA, Granoff DP, Park EY. Brown recluse spider bite: two case reports and review. J Am Podiatr Med Assoc 1998;88: 37-41. [DOI] [PubMed] [Google Scholar]
- 4.Vetter RS. Envenomation by a spider, Agelenopsis aperta (family: Agelenidae), previously considered harmless. Ann Emerg Med 1998;32: 739-741. [DOI] [PubMed] [Google Scholar]
- 5.Russell FE. A confusion of spiders. Emerg Med 1986;18: 8-9, 13. [Google Scholar]
- 6.Russell FE, Gertsch WJ. For those who treat spider or suspected spider bites [letter]. Toxicon 1983;21: 337-339. [DOI] [PubMed] [Google Scholar]
- 7.Vetter RS, Visscher PK. Bites and stings of medically important venomous arthropods. Int J Dermatol 1998;37: 481-496. [DOI] [PubMed] [Google Scholar]
- 8.Rosenstein ED, Kramer N. Lyme disease misdiagnosed as a brown recluse spider bite [letter]. Ann Intern Med 1987;107: 782. [DOI] [PubMed] [Google Scholar]
- 9.Sonenshine DE. The Biology of Ticks. Vol 2. New York: Oxford University Press; 1993.
- 10.Moaven LD, Altman SA, Newnham AR. Sporotrichosis mimicking necrotising arachnidism [letter]. Med J Aust 1999;171: 685-686. [DOI] [PubMed] [Google Scholar]
- 11.Fisher RG, Kelly P, Krober MS, Weir MR, Jones R. Necrotic arachnidism. West J Med 1994;160: 570-572. [PMC free article] [PubMed] [Google Scholar]
- 12.Krinsky WL. Envenomation by the sac spider Chiracanthium mildei. Cutis 1987;40: 127-129. [PubMed] [Google Scholar]