Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Vanessa Ngan, Staff Writer, 2003. Updated by Dr Malini Sivasaththivel, RMO, Eastern Health, Box Hill, Australia; Dr Smriti Tandon, Dermatology Registrar, Eastern Health, Box Hill, Australia; Dr Lena Ly, Dermatologist, Eastern Health, Box Hill, Australia. Copy edited by Gus Mitchell. January 2021.
" data-index="1" alt="Go to Introduction
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(1 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Introduction
" data-index="2" alt="Go to Demographics
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(2 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Demographics
" data-index="3" alt="Go to Causes
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(3 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Causes
" data-index="4" alt="Go to Clinical features
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(4 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Clinical features
" data-index="5" alt="Go to Dermoscopic features
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(5 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Dermoscopic features
" data-index="6" alt="Go to Complications
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(6 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Complications
" data-index="7" alt="Go to Diagnosis
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(7 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Diagnosis
" data-index="8" alt="Go to Differential diagnoses
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(8 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Differential diagnoses
" data-index="9" alt="Go to Treatment
" onclick="event.preventDefault();document.getElementsByTagName('h2')[(9 - 1)].scrollIntoView({behavior: 'smooth',block: 'start'});">Treatment
Outcome
Pyogenic granuloma is an acquired benign proliferation of capillary blood vessels of the skin and oral cavity. The name is a misnomer as it is a form of lobular capillary haemangioma, not due to infection. Pyogenic granuloma has many synonyms including granuloma gravidarum or pregnancy tumour when occurring in pregnancy.

Pyogenic granuloma

Pyogenic granuloma

Pyogenic granuloma
Pyogenic granuloma often occurs in children around 6 years of age and during teenage and young adult life. There is an overall male predominance (3:2) except for oral lesions due to their association with pregnancy and oral contraceptive use. There is no racial predilection.
Factors associated with the development of a pyogenic granuloma may include:
Pyogenic granuloma of the skin presents as a painless red fleshy nodule, typically 5-10mm in diameter, that grows rapidly over a few weeks. The surface is initially smooth but can ulcerate, become crusty, or verrucous. Pyogenic granuloma is usually solitary, but multiple nodules and satellite lesions can erupt. The most common sites involved are the fingers and face. Pyogenic granuloma easily bleeds with minor trauma.
Oral mucosal pyogenic granulomas typically develop on the lip and gums (gingiva) as pedunculated or sessile slow-growing painless red papules ranging in size from a few millimetres to several centimetres. The surface can be ulcerated with a yellow-fibrinous surface, and easy bleeding. With time, the lesion becomes a paler pink colour. Other mucosal sites that can be affected include the conjunctiva and nasal mucosa.




New lesion

2 weeks later

4 weeks after first photograph
Pyogenic granuloma has a distinct keratinised border forming a white collarette. Vascular structures are usually present and there are red homogenous areas with no clear lacunar pattern. White linear ‘rail lines’ are an important feature.

Pyogenic granuloma dermoscopy
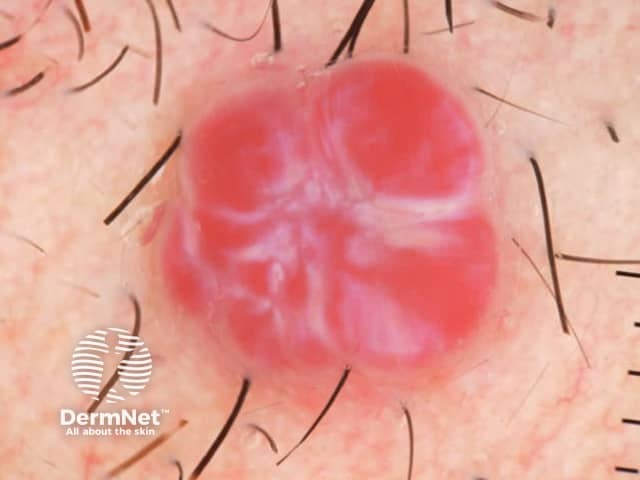
Red clods separated by white lines in pyogenic granuloma
Pyogenic granuloma can bleed profusely and frequently with minor trauma, resulting in anaemia.
Oral pyogenic granuloma can rarely cause significant bone loss.
Pyogenic granuloma is usually a clinical diagnosis. However, tissue may be submitted for histology following surgical treatment of the lesion or where there are concerns about the diagnosis.
Histology of pyogenic granuloma shows a prominent lobular capillary arrangement in the dermis. The overlying epidermis may be thinned or ulcerated, and the peripheral collarette is formed by elongated rete ridges and eccrine ducts. Inflammatory changes and signs of haemorrhage are secondary.

Dermal lobular arrangement of capillaries
There are two distinct histological types of oral pyogenic granuloma. In addition to the lobular capillary haemangioma pattern, a second type shows a distinct granulation tissue-like vascular proliferation which is postulated to have a different aetiology and evolution.
The clinical differential diagnosis of cutaneous pyogenic granuloma includes:
Amelanotic or hypomelanotic melanoma is the most important differential diagnosis even on dermoscopy with many shared features.
The differential diagnosis of oral cavity pyogenic granuloma includes the above, as well as the site-specific peripheral giant cell granuloma and peripheral ossifying fibroma.
The differential diagnosis on histology includes cherry angioma and bacillary angiomatosis.
Treating or removing triggering factors is important to minimise the risk of recurrence. This may include:
Pyogenic granuloma rarely resolves spontaneously except post-partum for lesions associated with pregnancy. Recurrence is common, especially for gingival lesions, after inadequate treatment or persistent aetiological factors.