Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Moushumi Das, Medical Registrar, Waikato Hospital, Hamilton, New Zealand. Editor-in-Chief: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. February 2016. DermNet Revision April 2021
Introduction Demographics Causes Clinical features Diagnosis Differential diagnoses Treatment Outcome
Benign lymphoplasmacytic plaque is a pseudolymphoma in children characterised by one or more chronic skin lesions, either solitary or in linear clusters, that have a characteristic polyclonal plasma cell infiltrate on histology. It was first described in 2009, with few reported cases so far.
Benign lymphoplasmacytic plaque has also been called cutaneous lymphoplasmacytic lymphoma and pretibial lymphoplasmacytic plaque.
Benign lymphoplasmacytic plaque has mostly been reported to affect female children between the ages of 7 and 15 years. Isolated cases have been described in adult males over the age of 60. It seems to predominantly affect people of Caucasian descent, although cases have also been described in Japanese, African, and South Asian (Indian) children.
The cause of benign lymphoplasmacytic plaque is unknown. Preceding trauma to the affected area has been noted in a few cases, but no direct correlation has been confirmed.
Benign lymphoplasmacytic plaque presents as a solitary chronic, persistent, and asymptomatic skin lesion that is resistant to topical and systemic treatment. Clusters of similar lesions often in a linear pattern may occur.

Lymphoplasmacytic plaque
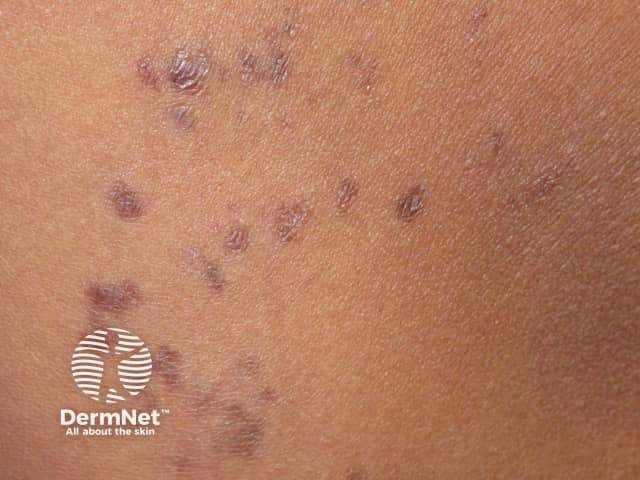
Lymphoplasmacytic plaque

Lymphoplasmacytic plaque: dermatoscopy
A skin biopsy is required as the diagnosis of benign lymphoplasmacytic plaque is made by dermatopathology and clinicopathologic correlation. The defining, compulsory histological findings are:
Epithelioid granulomas may be seen.
Other tests should be performed to rule out infections, specifically atypical mycobacteria, leishmaniasis, borreliosis, syphilis, and fungal infections. The plasma cells must be tested for clonality to exclude the possibility of a lymphoproliferative disorder.
Benign lymphoplasmacytic plaque can be removed by surgical excision. Topical steroids and systemic steroids, intralesional steroid injection, partial removal by shave excision, and oral antibiotics have not proved successful.
It is uncertain how benign lymphoplasmacytic plaque progresses long term. Two cases persisting for ten years have been reported with no clinical changes. Spontaneous regression have not been reported.