Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: AJ Sykes, Medical Registrar, Auckland City Hospital, Auckland, New Zealand. Editors: DermNet New Zealand Editor in Chief, Amanda Oakley, Dermatologist, Hamilton, New Zealand; Peter Storey, Clinical Immunologist and Allergy Specialist, Auckland City Hospital, Auckland, New Zealand. Copy editor: Maria McGivern. March 2017.
Introduction Allergy vs. intolerance Type I hypersensitivity reaction Type II hypersensitivity reaction Type III hypersensitivity reaction Type IV hypersensitivity reaction
Allergy is an abnormal response of the body to a foreign body, known as an antigen. It involves the immune system recognising this antigen and mounting one of four types of response, which are detailed below.
Allergy is also known as a ‘hypersensitivity reaction’ or a ‘hypersensitivity response’.
This article uses the terms allergy and hypersensitivity interchangeably. An allergy refers to the clinical syndrome while hypersensitivity is a descriptive term for the immunological process.
Intolerance refers to an individual’s ability to handle different types of food or drink. Food intolerance is not a true allergy, in that there is no clearly defined immune response and the symptoms that often develop only affect the digestive tract. An intolerance is normally found in the context of a deficiency in certain enzymes that break down the components of food. The absence of these enzymes thus results in abnormal byproducts that produce the symptoms of intolerance.
In contrast, a true allergy tends to affect multiple organ systems within the body and tends to have a poorer outcome.
A good example of the difference between an allergy and food intolerance can be made by comparing coeliac disease, an allergy, with lactose intolerance.
Type I hypersensitivity reaction is the most widely known type of allergic reaction and includes anaphylaxis; this is where the body reacts to a stimulus, or allergen, leading to swelling of the airways, and cardiovascular and other organ system effects. True anaphylaxis is uncommon.
Anaphylaxis occurs when a specific type of antibody, immunoglobulin E (IgE), recognises a foreign antigen and attaches itself to it. By attaching to the antigen, the IgE activates a chain of reactions that result in the widespread release of chemicals, including histamine.
Type I hypersensitivity reactions include:
The symptoms of a type I hypersensitivity reaction include:

Angioedema

Urticaria
The diagnosis of type I hypersensitivity reactions is largely based on the patient’s clinical history of typical symptoms and signs following exposure to a particular allergen. Tests can aid in confirming the diagnosis.
Anaphylaxis is a medical emergency requiring prompt recognition and treatment. Treatment of type I hypersensitivity reactions include:
People with known anaphylaxis to common environmental triggers (eg, bee venom or peanuts) may carry a pre-loaded adrenaline syringe or an adrenaline pen (eg, an EpiPen) that allows the rapid and easy injection of adrenaline into the thigh muscle in an emergency.
Desensitisation can be performed by an allergy specialist (an immunologist with interest in allergy) within the hospital environment. It involves gradually exposing the patient to increasing doses of the allergen (eg, an antibiotic) in an attempt to desensitise the patient’s immune response.
Type II hypersensitivity reactions, or autoimmune reactions, are due to the abnormal binding of antibodies to normal host targets. Autoimmune diseases involve immunoglobulin G (IgG) and M (IgM) antibodies that activate the complement cascade. This causes inflammation and damage to tissues.
The complement cascade forms part of the innate immune system that fights infection. The innate immune system always responds in the same way to a foreign stimulus and does not change or adapt over time. When exposed to a foreign protein, the complement cascade activates the adaptive immune system to form antibodies. Over time, the antibodies remember the foreign protein and clear foreign invaders (eg, bacteria and viruses) and damaged cells. It is a self-amplifying cascade of enzyme activation: downstream enzymes act to further increase the level of activation of the upstream enzymes, thereby increasing the response.
Cutaneous examples of type II hypersensitivity reactions include:
The diagnosis of a type II hypersensitivity reaction is confirmed by detecting causative antibodies. Direct immunofluorescence is used in skin biopsies of the skin adjacent to blisters to detect bullous pemphigoid and pemphigus vulgaris.

Bullous pemphigoid

Pemphigus vulgaris
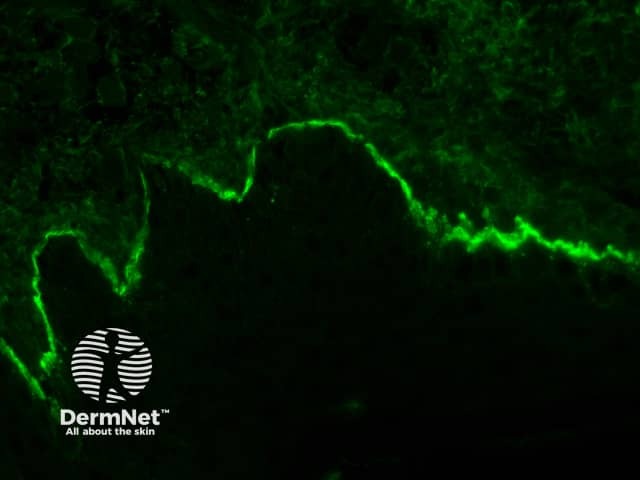
Direct immune fluoroescence
Currently, immunosuppression is the mainstay of treatment to prevent the action of abnormal antibodies.
Type V hypersensitivity is a relatively newly described reaction in which an antibody targets receptors on the cell surface that are normally activated by hormones. It is likely a subset of type II hypersensitivity reactions, as it involves an antibody targeting a specific structure within the body, leading to the clinical syndrome through abnormal cell signalling, either through the antibody activating a receptor or through blocking the binding of the normal hormone. No dermatological type V hypersensitivity reactions have been described.
Common non-cutaneous examples of type V hypersensitivity reaction include:

Graves disease
Type III hypersensitivity reaction involves IgG antibodies bound to foreign antigens in the blood. These antibody–antigen complexes can precipitate and get stuck in certain locations, such as blood vessels in the skin, kidneys and joints, where they activate the complement cascade to cause local damage.
Common cutaneous examples of type III hypersensitivity reactions include:
Most commonly, immune-complex reactions cause palpable purpura, the hallmark of small-vessel vasculitis. These are visible, non-blanching haemorrhages that are raised and palpable on examination.

Small vessel vasculitis

Systemic lupus erythematosus

Rheumatoid nodules
There are a large variety of diseases that can lead to type III hypersensitivity reactions. The appropriate tests are dictated by the patient’s clinical history and examination. There is no single test that can identify the cause of the hypersensitivity reaction.
Punch biopsies of the vasculitis rash typically show a leukocytoclastic reaction, in which there is superficial and mid perivascular neutrophilic infiltration with fibrinoid necrosis of the vessels and fibrin extravasation.
The treatment for type III hypersensitivity reactions is aimed at controlling the underlying disease. It often involves immunosuppression with systemic glucocorticoids and disease-modifying drugs, such as methotrexate, ciclosporin and cyclophosphamide.
Type IV hypersensitivity or delayed hypersensitivity reaction occurs 48–72 hours after exposure to the allergen. This reaction does not involve antibodies. Instead, eosinophils, monocytes, or lymphocytes called T cells are activated by the antigen. The helper CD4+ T cells initially recognise the antigen, releasing cytokines that activate the immune system with killer CD8+ T cells to destroy the target cells on contact, and macrophages to wall off the antigen and prevent further damage.
Common examples of cutaneous type IV hypersensitivity reactions include:

Morbilliform drug reaction

Lichenoid drug eruption

Toxic epidermal necrolysis
A thorough history and examination are required to identify the likely causative agent when considering a possible allergic contact dermatitis. Diagnosis is confirmed through patch testing (also known as a contact delayed hypersensitivity allergy test).
The mainstay of treatment for type IV hypersensitivity reactions is the avoidance of contact with the causative agent. For example, people with nickel allergy should select jewellery and clothing items that do not contain the metal.
Symptomatic relief of contact dermatitis is achieved through emollients and topical steroids.
Systemic corticosteroids are prescribed for severe reactions and tapered over 2–3 weeks to prevent a recurrence of the rash.
Monoclonal antibodies are antibodies generated within a laboratory setting that can be directed against the abnormal antibodies or cells in an affected individual. They can be directed against very specific molecules, allowing for specific targeting within a disease pathway. Monoclonal antibodies can be used in treating hypersensitivity reactions.
Omalizumab is an anti-IgE antibody, and therefore can be used in treating type I hypersensitivity reactions. It has been shown to have benefit in patients with moderate-to-severe asthma. Its use in other allergic conditions is also being studied.
Rituximab is an anti-CD20 monoclonal antibody that is helpful in treating type II and III hypersensitivity reactions. Rituximab is directed against the CD20 molecule found on the surface of B cells that produce antibodies. The rituximab acts as a signal for natural killer cells within the blood to target B cells and destroy them, reducing the level of abnormal antibody production seen in type II and III hypersensitivity reactions.
Anti-complement monoclonal antibodies are antibodies directed against certain components within the complement cascade. These biologic agents are already in use for several immunological diseases and are being investigated in hypersensitivity reactions.