Abstract
Objective
The study sought to identify smartphone apps that support hand hygiene practice and to assess their content, technical and functional features, and quality. A secondary objective was to make design and research recommendations for future apps.
Materials and Methods
We searched the UK Google Play and Apple App stores for hand hygiene smartphone apps aimed at adults. Information regarding content, technical and functional features was extracted and summarized. Two raters evaluated each app, using the IMS Institute for Healthcare Informatics functionality score and the Mobile App Rating Scale (MARS).
Results
A total of 668 apps were identified, with 90 meeting the inclusion criteria. Most (96%) were free to download. The majority (78%) intended to educate or inform or remind users to hand wash (69%), using behavior change techniques such as personalization and prompting practice. Only 20% and 4% named a best practice guideline or had expert involvement in development, respectively. Innovative means of engagement were used in 42% (eg, virtual or augmented reality or geolocation-based reminders). Apps included an average of 2.4 out of 10 of the IMS functionality criteria (range, 0-8). The mean MARS score was 3.2 ± 0.5 out of 5, and 68% had a minimum acceptability score of 3. Two had been tested or trialed.
Conclusions
Although many hand hygiene apps exist, few provide content on best practice. Many did not meet the minimum acceptability criterion for quality or were formally trialed or tested. Research should assess the feasibility and effectiveness of hand hygiene apps (especially within healthcare settings), including when and how they “work.” We recommend that future apps to support hand hygiene practice are developed with infection prevention and control experts and align with best practice. Robust research is needed to determine which innovative methods of engagement create “sticky” apps.
Keywords: smartphone, mobile health, review, hand hygiene, hand washing, infectious diseases
INTRODUCTION
Background and significance
According to the World Health Organization,1 good hand hygiene is one of the most simple but effective means of preventing the transmission of harmful microbes and acquirement of healthcare-associated infections. The severe acute respiratory syndrome coronavirus 2, causing the COVID-19 (coronavirus disease 2019) pandemic, further reenforces the need for good hand hygiene practice, both within healthcare settings and in everyday life.2
Daily good hand hygiene practice should include washing hands with clean water and soap before and after eating, handling raw meat or vegetables, changing a nappy, and treating a wound and after using the toilet and touching animals, and whenever hands feel or look dirty.3 In healthcare settings, the World Health Organization (WHO) recommendations for 5 Moments for Hand Hygiene include hand washing before and after touching a patient, after (risk to) exposure to bodily fluids, before clean or aseptic procedures, and after touching patient surroundings.4 The WHO 11 steps is an example of guidance on the correct hand hygiene technique.5 This includes wetting hands with water, applying soap, rubbing palms, interlacing fingers and then rubbing palms, cleaning the back of fingers by interlocking fingers, rotational rubbing of thumbs, rinsing hands with water, drying them thoroughly, and using a towel to turn off the faucet. Other techniques (eg, WHO 6 steps) combine or exclude some of the steps (eg, turning off the faucet).
Despite the presence of well-established guidelines, adherence to best practice hand hygiene by the general public and patients is suboptimal. Evans et al6 found that 90% of 100 adults did not wash their hands appropriately after handling raw chicken. In addition, microorganisms of fecal origin have been found on the hands of one-quarter of adults in the general population, indicating low compliance of hand hygiene after using the toilet.7 Randle et al8 observed a 56% and 57% hand hygiene compliance rate for hospitalized patients and their visitors, respectively.
Studies on hand hygiene in health and care staff showed similar room for improvement: home care (community) nurses were found to have an average adherence rate of 45.6%9 and nurses working in intensive care units (ICUs) of 52%.10 A systematic review of literature pertaining to student nurses concluded that hand hygiene knowledge and compliant behavior was low to moderate.11 Another review synthesized 61 studies in ICU settings and found that mean hand hygiene compliance by staff was 59.6%.12 However, this differed by type of ICU, geographic region, and healthcare workers (nursing staff 43.8% and physicians 32.6%). Erasmus et al13 also reported a higher adherence rate for nurses compared with physicians (48% and 32%, respectively) in their review on healthcare workers, with overall median compliance rate being 40%. This may be because doctors have been shown to perceive hand hygiene as important for protecting themselvesbut not for protecting their patients,13 as reflected by better compliance after having direct contact with a patient (55.1%) than before (38.4%).14
While barriers to hand hygiene in general adults have not been extensively researched, many factors explain why health and care providers do not hand wash appropriately.15–18 These barriers are related to awareness, familiarity, agreement, self-efficacy, outcome expectancy, the inability to overcome the inertia of previous practice, and external barriers.19 For example, a lack of knowledge of hand hygiene protocols can be explained as a lack of awareness and familiarity with guidelines. Additionally, skepticism and the belief that gloves are sufficient align with the lack of agreement with best practice guidelines and of outcome expectancy. External barriers may include limited hand hygiene training and training that is too theoretical and passive.14,20
Interventions aiming to improve hand hygiene compliance in health and care staff and general adults have been evaluated and include monitoring and providing performance feedback, electronic reminders, workshops, educational campaigns, and using cues (eg, visual posters or examining disinfected hands under ultraviolet lights).18,21–24 These mostly address barriers related to lack of awareness, overcoming inertia of previous practice, and improving self-efficacy.
Interactive and engaging digital interventions may help to overcome some of the barriers to hand hygiene. Primarily, mobile apps can be more affordable than traditional hand hygiene interventions (estimatedto be £146-£3035 when accounting for staff time and resources).23 When compared with automated monitoring systems,25,26 smartphone apps can monitor instances within communities and provide feedback on technique. In addition, they do not require significant financial investment and can provide educational material, which is recommended in adjunct to monitoring systems.26 Interventions delivered on mobile devices can also be creative, less time consuming, use multiple behavior change strategies, and be continuously available (eg, at home), so they may reinforce habitual behavior to help overcome engrained previous practice and change perceptions or attitudes (eg, skepticism).27 However, many digital interventions experience poor uptake, and very few are “sticky” (ie, enjoyable to use and engaging). While it is unknown as to what exactly makes technologies sticky,28 some expected characteristics include being intuitive, accessible, engaging, motivational, personalizable, and providing triggers, such as external cues or reminders.29,30 Smartphones naturally incorporate some of these aspects. For example, mobile apps are easily accessible, making them ideal for behavior change by using techniques such as self-monitoring, goal setting, increasing awareness or familiarity, and improving self-efficacy.
Previous research has already compared which technologies may help to improve hand hygiene compliance31 and has identified that mobile apps may be an appropriate new way of addressing suboptimal hand hygiene.32,33 However, the app market is saturated with health apps, with over 318 000 available in 2018 and an additional 200 added daily.34 Many of these have not been formally evaluated nor developed with experts, creating concern about the extent to which they distribute reliable health information and, in the case of hand hygiene, encourage good practice.
OBJECTIVE
The objective of this review is to provide an overview of what hand hygiene mobile apps are currently available and to assess their content, technical and functional features, and quality. A secondary objective is to make recommendations for the future development of similar apps.
MATERIALS AND METHODS
We conducted a systematic review and content analysis of hand hygiene mobile apps in line with previous app reviews.35–39 Where relevant, the review was reported in alignment with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.40
Search strategy and inclusion criteria
While the target audience of this review was intended to be healthcare providers, an initial scoping search highlighted that few apps specified their intended users. App markets do also not enable for categorization of target users, unless they are children. Therefore, we included apps aimed at adults in general.
We identified apps on November 19, 2020, from 2 UK app markets (App Store and Google Play) using the keywords hand hygiene and hand washing. Apps that focused on hand hygiene (hand washing or sanitation) and targeted at adults were included in the review. Those aimed at children, groups or organizations (rather than individuals), and particular health hygiene issues other than hand hygiene (eg, wearing masks to protect against COVID-19) or those not in English were excluded.
App selection
A 2-step screening process was conducted. First, 1 author (N.G.) screened the app markets for relevant apps by looking at their titles and descriptions. Duplicates between the app markets were removed. Second, 3 authors (N.G., S.M.A., A.J.S.S.) downloaded the apps to confirm their eligibility. Two authors reviewed the apps in the Google Play store (N.G. and S.M.A.) and 2 in the App store (N.G. and A.J.S.S.). The iPhone SE (iOS 13.6.1), iPhone 7 (iOS 14.2), Samsung Galaxy J6 (Android v8.0 Oreo), and Samsung Galaxy S20 FE (Android v10.0) devices were used. Some apps required additional devices, so we also used the Xiaomi Mi Smart Band 4 and the Destek V5 virtual reality headset.
Data extraction
Two authors independently assessed the functionality and quality of each app and recorded relevant information on a data extraction sheet in Excel. This included descriptive information, content, technical and functional features, and quality (see Supplementary Table 1 for a summary of the data extraction items).
Table 2.
Summary of the included hand hygiene mobile apps (n = 90)
| General characteristics | |
| Purchase costs | |
| Free to download | 75 (83) |
| Free to download with in-app purchases | 11 (12) |
| Costs to download | 4 (4) |
| Affiliated with a health/medical body | |
| Yes | 4 (4) |
| No | 86 (96) |
| Named a best practice hand hygiene guideline | |
| Yes | 18 (20) |
| No | 72 (80) |
| Had a privacy strategy (eg, login, policy) | |
| Yes | 70 (78) |
| No | 20 (22) |
| Used an innovative means of engagement | |
| Yes | 38 (42) |
| No | 52 (58) |
| App quality (MARS scores) | |
| Overall quality score | 3.2 ± 0.5 |
| Engagement | 2.7 ± 0.7 |
| Functionality | 4.2 ± 0.5 |
| Aesthetic | 3.3 ± 0.7 |
| Information quality | 2.6 ± 0.6 |
Values are n (%) or mean ± SD.
MARS: Mobile App Rating Scale.
The descriptive information included the name of the app, the version number, the developer, the market(s) in which the app was available, the cost, whether the app was affiliated with a professional body, the average user rating, and the number of ratings.
We explored content by identifying the purpose of each app and common behavior change techniques it employed. The behavior change techniques included self-monitoring, feedback, goal setting, social support, reward or threat, prompting practice, or personalization.41–43 These were the most commonly reported behavior change strategies used in mobile apps, as identified by Taj et al44 and Dugas et al.45 Other content-related information included whether the app mentioned aligning with any best practice hand hygiene guidelines and the comprehensiveness of the content.
To assess the comprehensiveness of the content, we developed common criteria from reputable sources and guidelines on hand hygiene3–5,46,47 and determined whether or not these were present in each app. Similar methods were used by Lalloo et al48 and Grainger et al.37 The 4 criteria were (1) context (eg, when to hand wash as in the WHO 5 Moments for Hand Hygiene, or for the general public after sneezing or using the toilet, and before eating), (2) use of soap or hand sanitizer (when soap is not available), (3) specific overall timing and length of hand wash (eg, 15-60 seconds), and (4) skill (eg, the WHO 11 steps to hand washing).
We also extracted information on technical and functional features. Technical features included whether the app had a privacy strategy (eg, policy, login, 2-factor authentication) and whether it used innovative features. We considered features innovative if they used any of the following technologies: geolocation tracking (eg, GPS), virtual or augmented reality, virtual assistants (eg, Siri), smartwatches (eg, Wear OS or Apple Watch), personal profiles, or gamification (eg, scores, competition or characters). Other information included whether it worked offline or specifically asked the user to work in the background or enable push notifications.
As in some other mobile app reviews,49,50 functionality was assessed using the IMS Institute for Healthcare Informatics functionality score.51 It consists of 7 criteria and 4 subcategories (see Table 1), rated 1 if they apply or 0 if they do not apply. We removed the item “evaluate data” because it pertains to whether the entered data can be evaluated by patient or provider, provider or administrator, or patient or caregiver, which was not relevant to the apps in our review. A total score was generated by summing the items, with a maximum score of 10. Reviewers resolved disagreements through discussion.
Table 1.
IMS Institute for Healthcare Informatics functionality score criteria and descriptions
| Functionality Scoring Criteria | Description |
|---|---|
| 1. Inform | Provides information in a variety of formats, eg, text, photo, video |
| 2. Instruct | Provides instructions to the user, eg, app use guides, instructions to interpret charts |
| 3. Record | Captures user-entered data, eg, hand washing log or score or location for where (or not) to hand wash |
| 3.1 Collect data | Able to enter and store health data on individual phone, eg, steps taken, location |
| 3.2 Share data | Able to transmit health data, eg, export, upload, or email data |
| 3.3 Intervene | Able to send alerts based on the data collected or propose behavioral intervention or changes, eg, hand washing alarm based on users’ data, hand washing reminder when movement or step count is detected |
| 4. Display | Graphically display user-entered data/output user-entered data, eg, hand hygiene trends chart |
| 5. Guide | Provide guidance based on user-entered information, and may further offer further help, eg, recommendations for improving technique or frequency of hand hygiene based off user data |
| 6. Remind or alert | Provide reminders to the user, eg, hand hygiene notifications |
| 7. Communicate | Provide communication between users, consumers or others and/or provide links to social networks, eg, in-app community or upload hand washing data to Facebook |
The criterion “evaluate data” was removed, as it was not relevant to the apps in our review.
In line with previous mobile app reviews,35,37–39 quality was assessed using the 19-item Mobile App Rating Scale (MARS).52 Items were rated on a 5-point Likert scale (1 = inadequate, 2 = poor, 3 = acceptable, 4 = good, and 5 = excellent), with items categorized into 4 dimensions: engagement, functionality, aesthetics, and information quality. Each author independently rated each dimension and calculated an overall mean score. A mean score between both reviewers was then calculated. A question in the scale asks, “Has the app being trialed/tested?,” which we answered by searching for empirical published literature that evaluated the app. This included evaluations for effectiveness, acceptability, usability, or satisfaction.
MARS also provided an optional subscale for subjective quality. However, as consistent with previous reviews, this scale was omitted to ensure that the quality assessments were consistent and objective across the reviewers.35,38,39 Reviewers watched the MARS training video on YouTube53 prior to rating.
Data synthesis
We synthesized the data descriptively. Where applicable, we generated descriptive summary statistics. The highest-scoring apps across the functionality and quality measures were identified and cross-compared, in order to identify the best overall apps.
To assess interrater reliability of the MARS scores, we calculated the intraclass correlation coefficients (ICCs) on all MARS items, using a 2-way mixed-effects, average-measures model with absolute agreement.54 For the IMS Institute for Healthcare Informatics functionality score, we calculated Cohen’s kappa, as ratings were categorical (0 = no, 1 = yes). All statistical analyses were conducted using IBM SPSS Statistics (version 23; IBM, Armonk, NY).
RESULTS
Figure 1 shows that the search yielded 668 apps. After screening the name and description of each app, and removing 6 duplicates, a total of 110 apps were downloaded and assessed. Of these, 20 were excluded, mostly owing to not being compatible with the devices (n = 7) or not opening (eg, crashing) (n = 6). A total of 90 apps were included in this review. Table 2 provides an overall summary of the apps.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart showing app identification and screening process.
Descriptive characteristics
Most of the apps (n = 86 of 90, 96%) were free to download, with 11 offering in-app purchases. The costs for paid apps ranged from £0.89 to £3.99. At the time of this review, 24 apps had been rated by between 1 and 249 users. Ratings ranged from 2.5 to 5 stars (out of 5). Most of the apps (n = 86 of 90, 96%) were not affiliated with a professional health or medical body, and only 4 said that they had been developed in partnership with infection prevention and control (IPC) expert groups, hospitals, universities, or behavioral scientists. Supplementary Table 2 lists and summarizes the included apps.
Hand hygiene content
The purpose of the included apps was to educate, instruct, or inform users on hand hygiene (eg, importance or skill) (n = 70 of 90, 78%), remind them to practice hand hygiene (n = 62 of 90, 69%), track their hand washing instances (eg, through a log) (n = 27 of 90, 30%), provide feedback (eg, on their performance or technique) (4 of 90, 4%), or convince them (through hypnosis) (n = 1 of 90, 1%).
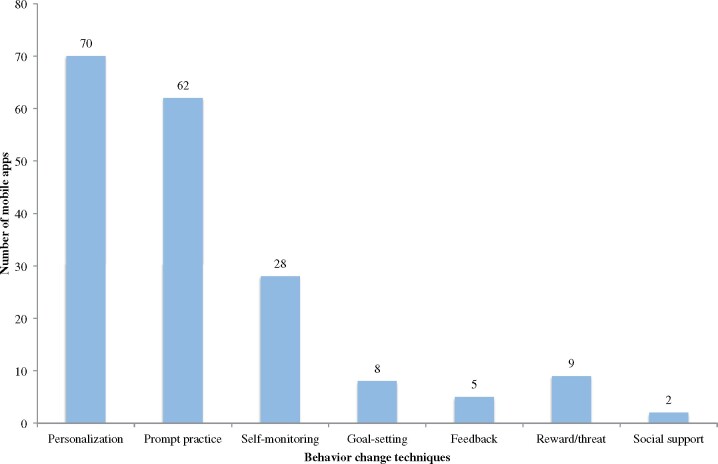
Apps used a range of established behavior change techniques, with an average of 2 techniques per app (range, 0-5). Thirteen (14%) did not use any of the behavior change techniques, 8 (9%) used 1 technique, 45 (50%) used 2 techniques, 13 (14%) used 3 techniques, 8 (9%) used 4 techniques, and 3 apps (3%) used 5 techniques. Figure 2 presents the frequency of each technique.
Figure 2.
Bar graph showing frequency of each behavior change technique used across included apps.
Across the apps, the most commonly used technique was personalization (n = 70 of 90, 78%) whereby users received personalized feedback or could change settings within the app. This included setting their reminder times, frequencies, sounds or music, notifications, or setting the language and location. The second most common technique was prompting hand hygiene practice (n = 62 of 90, 69%), as evident in all of the reminder apps.
Self-monitoring (n = 28 of 90, 31%) was often used in the apps that intended to track hand washing instances or performance, and often included presenting a log or hand hygiene history that enabled users to monitor their progress. Some (n = 8 of 90, 9%) of the apps also used goal-setting strategies such as by calculating the number of hand washing instances that should be achieved within a specified timeframe. This goal was then presented to the user and they could monitor their instances against it.
Feedback (n = 5 of 90, 6%) was used less often but included giving users a summary of their performance (eg, in games) or of their technique. Similarly, reward or threat were less commonly used (n = 9 of 90, 10%) but were usually employed in games through scores (as reward) or loss of points or “lives/hearts” (as a threat). Reward was also used when goals were met, such as by enabling the user to move up a level or change a function in the app. Very few (n = 2 of 90, 2%) of the apps facilitated social support (eg, encouraging users to share their data or progress to social media).
Although many of the apps intended to educate or inform users, not many drew on best practice hand hygiene guidelines. Specifically, only 20% (n = 18 of 90) named a guideline. Steps for how to practice hand hygiene were named the most (n = 15), compared with guides on when to hand wash (n = 7) or general guidelines for IPC (n = 2). Guidelines for practicing hand hygiene included the WHO 6, 10, or 11 Steps to Hand Washing (n = 8); Centers for Disease Control and Prevention (CDC) guides for hand washing (n = 6); or the NHS 11 Steps to Hand Wash (n = 1). Guidelines for when to hand wash mostly included the WHO 5 Moments for Hand Hygiene (n = 5), a general WHO guide for when to hand wash (n = 1), and a CDC guide for when to hand wash (n = 1). The 2 IPC guidelines named were the CDC guide for Infection Control and the WHO general guideline for preventing the transmission of diseases.
Four criteria were used to assess the comprehensiveness of the hand hygiene content. Of the included apps, 14 (16%) did not mention any criteria, 26 (29%) mentioned 1 criterion, 9 (10%) apps mentioned 2 criteria, 28 (31%) mentioned 3 criteria, and 13 (14%) mentioned all 4 criteria. Length of practice was included the most (n = 63 of 90, 70%), followed by use of soap or sanitizer (n = 54 of 90, 60%), skill (n = 47 of 90, 52%), and context (n = 15 of 90, 17%).
Technical features
Of the apps, 83% (n = 75 of 90) worked offline and 7% (n = 6 of 90) asked the user whether it could work in the background. Although 62 of the apps sent reminder notifications to users, 47 (78%) of these asked users to enable push notifications. Some included a privacy policy (n = 19 of 90, 21%) or a login of password (n = 3 of 90, 3%). However, none offered 2-factor authentication and most (n = 70 of 90, 78%) did not include any privacy strategies.
Innovative means of engagement were used in 42% (n = 38 of 90) of the apps, including geolocation or movement-based reminders (n = 13 of 90, 14%), gamification (n = 10 of 90, 11%), personal profiles (n = 10 of 90, 11%), interfaced with smartwatches (n = 5 of 90, 6%), virtual assistants (eg, Siri) (n = 4 of 90, 4%), augmented reality (n = 3 of 90, 3%), and virtual reality (n = 1 of 90, 1%). Table 3 provides examples of how apps implemented these features.
Table 3.
Examples of innovative technical features used within some of the apps
| Feature | Example of how apps implemented the feature |
|---|---|
|
|
| Personal profiles | Users can create personal profiles in HandAssure and StatWash by inputting information such as their name, age, and gender. In some apps, they can link their existing profiles (eg, social media or Google accounts) to also use their photographs. Other apps ask for weight, daily workout time, wake up and bed times, personal hand hygiene goals, and workplaces. |
| Smartwatches | In the LatherApp Hand Wash Timer app, users can connect hand hygiene reminders to their smartwatch. This means that they do not touch their phone when receiving a reminder. |
| Use of virtual assistants | In a karaoke-style app Happy Wash, users are encouraged to sing along to the happy birthday song while hand washing. They can create shortcuts to Siri, to activate the hand washing timer and song. |
| Augmented reality |
|
| Virtual reality and gamification | Users wear a virtual reality headset to become immersed in the Tork VR Clean Hands Training game. They are shown how to perform hand hygiene properly and select a character (nurse or doctor). During their shift, they must care for patients. The nurse provides care (eg, adjusting patients, administering medication, taking blood pressure and hemoglobin readings and dressing wounds). The doctor performs diagnoses and examinations (eg, auscultating the heart and visual examination of urine). The user is guided through a “thought bubble.” They must perform hand hygiene at appropriate times (eg, before/after touching patient) and choose when to use gloves and how to appropriately dispose of them. Feedback is provided on missed opportunities. At the end of the shift, the user is debriefed with a summary of opportunities for hand hygiene, missed opportunities and overall compliance. |
Functionality
Functionality was assessed using 10 items from the IMS Institute for Healthcare Informatics functionality score. There was substantial agreement between the 2 raters’ scores of the Apple App Store apps (κ = .76; 95% confidence interval, .67-.85; P < .0000). Similarly, there was substantial agreement between the 2 raters in the Google Play Store (κ = .80; 95% confidence interval, .74-.86; P < .0000). Absolute agreement was reached through discussion.
Figure 3 shows that the most common functions were the ability to inform users on hand hygiene (n = 62 of 90, 69%), provide reminders or alerts (eg, push notifications) (n = 61 of 90, 68%), and record data (eg, hand washing scores) (n = 34 of 90, 38%). Overall, apps had an average of 2.4 (out of 10) functions (range, 0-8) (see Supplementary Table 2). Only 1 app (SureWash Hand Hygiene Pro) had 8 functions, followed by 3 apps (Tork VR Clean Hands Training, SureWash Hand Hygiene, and Remember Washing Your Hands—Handwashing Reminder) that had 7 functions. Three apps (Wash Stuff, Hand Wash Timer—Wash Your Hands For 20 Seconds, and Wash Hands Timer) had none of the functions. These apps tended to be simple hand wash timer or countdown apps.
Figure 3.
Functionality of the apps, using 10 items from the IMS Institute for Healthcare Informatics functionality score.
Quality
All apps were independently evaluated by 2 raters using MARS. The authors who reviewed the apps in the App Store had good interrater reliability (ICC = .88; 95% confidence interval, .86-.90). Interrater reliability between the authors who reviewed the apps in the Google Play market was also good (ICC = .88; 95% confidence interval, .87-.90).
The mean overall quality score across the apps was 3.2 ± 0.5). Only 68% (n = 61 of 90) met the minimum acceptability score of 3.52 The best apps were rated 4.6 (SureWash Hand Hygiene; SureWash Hand Hygiene Pro) and the worst rated was 2.4 (Hand Wash Timer—Wash Your Hands for 20 Seconds). Mean scores for engagement, functionality, aesthetics, and dimensions were 2.7 ± 0.7, 4.2 ± 0.5, 3.3 ± 0.7, and 2.6 ± 0.6, respectively. Most apps (n = 84 of 90, 93%) scored highest on the functionality dimension and lowest on information quality (n = 50 of 90, 56%). Only 2 of the apps (SureWash Hand Hygiene and SureWash Hand Hygiene Pro) had been formally trialed or tested,55,56 but not in robust randomized controlled trial experiments. We reviewed the SureWash apps individually, as they are 2 different versions. Supplementary Table 3 summarizes the MARS scores for each app.
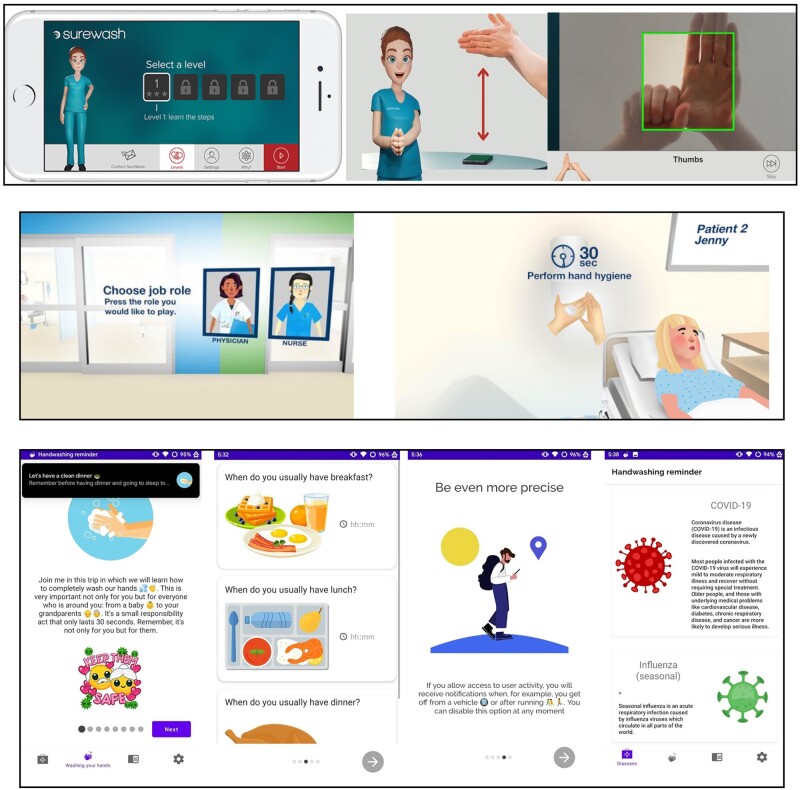
Overall app quality
The apps that had the highest IMS functionality and MARS scores were cross-compared. The highest-performing apps and their defining characteristics are highlighted in Table 4 and include SureWash Hand Hygiene Pro, SureWash Hand Hygiene, Tork VR Clean Hands Training, and Remember Washing Your Hands—Handwashing Reminder. Figure 4 provides images of each of these apps.
Table 4.
Highest-performing apps included in the review
| Name | Market, Cost | IMS Scorea | MARS Scoreb | Purpose | Innovative Technical Features | Behavior Change Technique |
|---|---|---|---|---|---|---|
| SureWash Hand Hygiene Pro |
Apple; Google Play £3.99 |
8 | 4.6 | Track, educate/instruct, provide feedback, remind | Augmented reality, gamification | Self-monitoring, feedback, reward, social support, personalization, prompt practice |
| SureWash Hand Hygiene |
Apple; Google Play free |
7 | 4.6 | Track, educate/instruct, provide feedback | Augmented reality, gamification | Self-monitoring, feedback, reward, social support, personalization |
| Tork VR Clean Hands Training |
Apple; Google Play free |
7 | 4.5 | Educate/instruct, provide feedback | Virtual reality, gamification | Self-monitoring, feedback, reward/threat, personalization |
| Remember Washing Your Hands—Handwashing Reminder |
Google Play free |
7 | 4.0 | Remind, track, educate/instruct | Tracking (log/chart), reminders (movement-based) | Self-monitoring, personalization, prompt practice |
MARS: Mobile App Rating Scale.
The IMS score refers to the overall score for the IMS Institute for Healthcare Informatics functionality score (range 0-10).
Overall mean MARS score.
Figure 4.
Images showing the highest scoring apps (from top to bottom): SureWash Hand Hygiene; SureWash Hand Hygiene Pro,57 Tork VR Clean Hands Training,58 and Remember Washing Your Hands—Handwashing Reminder.59
DISCUSSION
To our knowledge, this is the first study to formally identify hand hygiene smartphone apps and assess their quality, functionality, and content. We assessed 90 apps, of which most intended to educate, inform or remind users to hand wash, often using behavior change techniques such as personalization and prompting practice. Only a few apps named a best practice hand hygiene guideline or had expert involvement in their development. However, 42% used an innovative means of engaging users. On average, the apps used 2.4 functions and had a quality score of 3.2. Only 2 had been formally tested or trialed.
A previous review of apps for healthcare-associated infection prevention was conducted by Schnall and Iribarren32 but only included 2 hand hygiene apps. Our review showed that many hand hygiene apps exist but that they vary greatly in quality. Indeed, many did not meet the minimum acceptability criterion for quality. While this review included hand hygiene apps aimed at adults, it did highlight some that were specifically targeted at health and care providers. Five of the apps contained content on the WHO 5 Moments of Hand Hygiene, a guideline for hand hygiene within clinical healthcare settings. Overall the apps were fairly simple, providing few functions and related behavior change techniques. The lack of adherence to best practice hand hygiene guidelines (eg, when and how to practice hand hygiene) or of engagement with experts in their development meant that their content did often not align with best practice, nor did it meet our criteria for comprehensiveness. This was also reflected in the MARS, whereby more than half of the apps scored lowest on the information quality dimension.
However, it was evident that the smartphone platform enabled innovative approaches to engagement, including elements of gamification and “fun” to inform users, geolocation to send accurate reminders, or augmented and virtual reality to provide personalized and real-time feedback on technique. Apps including these innovative features addressed some of the common barriers to hand hygiene, including helping to improve self-efficacy in technique, combating forgetfulness and skepticism, and promoting awareness and familiarity of best practice guidelines.15–18 These engaging apps may also overcome external barriers such as training that is too theoretical and passive.14,20 In fact, the SureWash app had previously been evaluated for effectiveness in improving technique. SureWash was used daily by 47 university staff and students in a 4-week prospective cohort study.55 By the end of the study period, 81% had reached proficiency in their technique.
The included apps also used a range of behavior change techniques and approaches to improving hand hygiene. These are commonly employed in other mobile app interventions.44,45 Previous research explored whether common behavior change strategies were able to improve hand hygiene compliance. In a systematic review by Seo et al,18 11 studies used campaign and educational strategies. Ten of these significantly improved hand hygiene compliance after the intervention. Similar results were reported by Doronina et al,21 who evaluated the effectiveness of hand hygiene interventions for nurses and concluded that education and feedback strategies positively affected compliance rates. However, these rates decreased after 1 month. Reminders and feedback systems also improved compliance, although this varied throughout the day.
According to Huis et al,60 many hand hygiene interventions do not facilitate long-term and sustained behavior change because they only address knowledge, facilitation, and awareness. They argued that more effective interventions should also target attitude, self-efficacy, intention,60 education, reminders, feedback,18,61 goal setting, accountability, and reward incentives.23 In line with Huis et al’s suggestion, some of the included apps employed different strategies to target multiple barriers of hand hygiene. However, we cannot comment on their effectiveness, as none had been formally and robustly evaluated.
Additionally, it is important to acknowledge that smartphone apps alone cannot address all barriers to hand hygiene. For example, deeply engrained personal beliefs, previous training and environmental factors (eg, access to hand sanitizer, soap, or clean water) are not addressed. Developers often design apps with a certain target audience in mind, making it hard to account for the full—and heterogeneous—range of potential users and contexts (eg, community, home, and clinical settings). Integrating the apps into multimodal interventions that address other barriers and are tailored to the settings in which they are used may therefore be most effective in promoting hand hygiene.
Design and research recommendations
Research is warranted to assess the feasibility and effectiveness of hand hygiene apps (especially within healthcare settings), including when and how they “work” in improving self-efficacy, knowledge of guidelines, and compliance to best practice. This should be considered before additional effort is devoted to producing better hand hygiene apps. In addition, robust research and development of theory is needed to determine which innovative methods of engagement create “sticky” apps. This includes in-app methods (eg, gamification or augmented reality), external phone-based tools (eg, virtual assistants, geolocation or movement tracking), or additional external tools (eg, virtual reality headsets or smartwatches, such as in Samyoun et al).62 Future research should explore the impact of these methods on engagement, as well as what level and duration of engagement leads to changed hand hygiene behavior or increased awareness of the correct technique. This may differ between types of apps. For example, compared with educational apps, users may need to engage with reminder apps more frequently and for longer to change their behavior.
Currently, there are few apps that contain hand hygiene content that aligns with recommended best practice. There is therefore great opportunity to include IPC experts in developing apps, something that only few apps in this review mentioned. Collaboration between IPC experts and app developers will likely yield apps that contain high-quality, accurate, and comprehensive content. At the same time (or when including experts is not practical), the content may be derived from best practice guidelines. In addition to education, reminding and feedback, future apps should also target attitude, intention, and self-efficacy, to promote effective and sustained behavior change. These should use an adaptive “Just-in-Time” approach that accounts for time and context.63 For example, providing reminders when individuals reach a high-risk area (eg, workplace) or enabling users to postpone or disregard notifications to avoid intervention fatigue.
Strengths and limitations
Unlike other app reviews,32,36 we included apps that required additional devices (eg, smartwatches) or used innovative features (eg, virtual assistants). This enabled us to also explore innovative methods of engagement, even though we had to exclude some apps that depended on additional devices that were not compatible with the ones we had available. Another strength included using the IMS Institute for Healthcare Informatics functionality score, unlike most other app reviews. While the MARS52 focused on navigation, performance, gestural design, and ease of use, the IMS Institute for Healthcare Informatics functionality score51 focused on the broader scope of function in regard to abilities. This includes the ability to inform, instruct, record, display, guide, remind, and communicate information.
The main limitation of the study was that only apps available in the United Kingdom were included. This means that it is possible that hand hygiene apps developed and released privately or by researchers were not included. Apps reported in academic literature (but not currently available in app stores), released overseas, or in languagesother than English were also excluded.
CONCLUSION
This systematic review identified many hand hygiene mobile apps available across 2 UK app stores. Many of these were simple, with few functions, and did not meet the minimum acceptability criterion. It was concerning to see that while many attempted to inform users on how to practice hand hygiene, only few mentioned that input from IPC experts or best practice guidelines informed their development. This limited the information quality, accuracy, and comprehensiveness of their content. Before producing better hand hygiene apps, research should assess their feasibility and effectiveness (especially within healthcare settings), including when and how they “work.” Future developments of hand hygiene behavior change apps should partner with IPC experts and draw on best practice guidelines. Robust research and development of theory is needed to determine which innovative methods of engagement work. Ultimately, this may result in the development of sticky apps that are trustworthy in their content.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank Dr Tony Payton, Dr Pauline Whelan, and Charlotte Stockton-Powdrell for generously lending us the required devices.
DATA AVAILABILITY
No new data were generated or analyzed in support of this research.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest.
FUNDING
This work is funded by the National Institute for Health Research Applied Research Collaboration Greater Manchester. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
AUTHOR CONTRIBUTIONS
NG designed the study, with support from SNvdV, DD, and PW. NG, SMA, and AJSS reviewed the apps. NG analyzed the data and wrote the first draft of the manuscript. NG, SNvdV, DD, and PW participated in the interpretation of the study findings and the preparation of the manuscript. All of the authors approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online
REFERENCES
- 1.World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. 2009. https://www.who.int/gpsc/5may/tools/9789241597906/en/. Accessed November 17, 2020.
- 2.World Health Organization. Who Save Lives: Clean Your Hands in the Context of COVID-19. 2020. https://www.who.int/infection-prevention/campaigns/clean-hands/WHO_HH-Community-Campaign_finalv3.pdf. Accessed November 17, 2020.
- 3.NHS. Hand washing. 2019. https://www.nhs.uk/live-well/healthy-body/best-way-to-wash-your-hands/. Accessed November 17, 2020.
- 4.World Health Organization. Hand hygiene: why, how & when? 2009. https://www.who.int/gpsc/5may/Hand_Hygiene_Why_How_and_When_Brochure.pdf. Accessed November 18, 2020.
- 5.World Health Organization. Clean hands protect against infection. 2020. https://www.who.int/gpsc/clean_hands_protection/en/. Accessed November 18, 2020.
- 6.Evans E, Redmond E.. Behavioral observation and microbiological analysis of older adult consumers' cross-contamination practices in a model domestic kitchen. J Food Prot 2018; 81 (4): 569–81. [DOI] [PubMed] [Google Scholar]
- 7.Judah G, Aunger R, Schmidt W-P, et al. Experimental pretesting of hand-washing interventions in a natural setting. Am J Public Health 2009; 99 (S2): S405–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Randle J, Arthur A, Vaughan N.. Twenty-four-hour observational study of hospital hand hygiene compliance. J Hosp Infect 2010; 76 (3): 252–5. [DOI] [PubMed] [Google Scholar]
- 9.McDonald M, Brickner C, Russell D, et al. Observation of hand hygiene practices in home health care. J Am Med Dir Assoc 2020. Sep 15 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taneja J, Mishra B.. Promotion of successful hand hygiene practices in the intensive care units of a tertiary care hospital. J Patient Saf Infect Control 2015; 3 (3): 130–3. [Google Scholar]
- 11.Labrague L, McEnroe-Petitte D, van de Mortel T, et al. A systematic review on hand hygiene knowledge and compliance in student nurses. Int Nurs Rev 2018; 65 (3): 336–48. [DOI] [PubMed] [Google Scholar]
- 12.Lambe K, Lydon S, Madden C, et al. Hand hygiene compliance in the ICU: a systematic review. Crit Care Med 2019; 47 (9): 1251–7. [DOI] [PubMed] [Google Scholar]
- 13.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol 2010; 31 (3): 283–94. [DOI] [PubMed] [Google Scholar]
- 14.Musu M, Lai A, Mereu N, et al. Assessing hand hygiene compliance among healthcare workers in six intensive care units. J Prev Med Hyg 2017; 58 (3): E231–37. [PMC free article] [PubMed] [Google Scholar]
- 15.Erasmus V, Brouwer W, van Beeck E, et al. A qualitative exploration of reasons for poor hand hygiene among hospital workers: lack of positive role models and of convincing evidence that hand hygiene prevents cross-infection. Infect Control Hosp Epidemiol 2009; 30 (5): 415–9. [DOI] [PubMed] [Google Scholar]
- 16.Mathur P.Hand hygiene: back to the basics of infection control. Indian J Med Res 2011; 134 (5): 611–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneider J, Moromisato D, Zemetra B, et al. Hand hygiene adherence is influenced by the behavior of role models. Pediatr Crit Care Med 2009; 10 (3): 360–3. [DOI] [PubMed] [Google Scholar]
- 18.Seo H-J, Sohng K-Y, Chang SK, et al. Interventions to improve hand hygiene compliance in emergency departments: a systematic review. J Hosp Infect 2019; 102 (4): 394–406. [DOI] [PubMed] [Google Scholar]
- 19.Cabana M, Rand C, Powe N, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999; 282 (15): 1458–65. [DOI] [PubMed] [Google Scholar]
- 20.Essity Internal. Tork Healthcare Hand Hygiene Survey. 2018. https://cdntorkprod.blob.core.windows.net/docs-c5/292/259292/original/tork-healthcare-survey-2018.pdf. Accessed November 18, 2020.
- 21.Doronina O, Jones D, Martello M, et al. Systematic review on the effectiveness of interventions to improve hand hygiene compliance of nurses in the hospital setting. J Nurs Scholarsh 2017; 49 (2): 143–52. [DOI] [PubMed] [Google Scholar]
- 22.Gould D, Moralejo D, Drey N, et al. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev 2017; 9: CD005186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luangasanatip N, Hongsuwan M, Limmathurotsakul D, et al. Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis. BMJ 2015; (351): h3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawson A, Vaganay-Miller M.. The effectiveness of a poster intervention on hand hygiene practice and compliance when using public restrooms in a university setting. Int J Environ Res Public Health 2019; 16 (24): 5036–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blomgren P-O, Lytsy B, Hjelm K, et al. Healthcare workers' perceptions and acceptance of an electronic reminder system for hand hygiene. J Hosp Infect 2021; 108: 197–204. [DOI] [PubMed] [Google Scholar]
- 26.Masroor N, Doll M, Stevens M, et al. Approaches to hand hygiene monitoring: From low to high technology approaches. Int J Infect Dis 2017; 65: 101–4. [DOI] [PubMed] [Google Scholar]
- 27.Murray E, Hekler E, Andersson G, et al. Evaluating digital health interventions: key questions and approaches. Am J Prev Med 2016; 51 (5): 843–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carlo AD, Hosseini Ghomi R, Renn BN, et al. Assessment of real-world use of behavioral health mobile applications by a novel stickiness metric. JAMA Netw Open 2020; 3 (8): e2011978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petrie R. How to engage patients with sticky technology. 2015. https://www.datstat.com/2015/09/patient-engagement/engage-patients-technology. Accessed December 10, 2020.
- 30.Ritterband L, Gonder-Frederick L, Cox D, et al. Internet interventions: in review, in use, and into the future. Prof Psychol Res Pract 2003; 34 (5): 527–34. [Google Scholar]
- 31.Dawson C, Mackrill J.. Review of technologies available to improve hand hygiene compliance – are they fit for purpose? J Infect Prev 2014; 15 (6): 222–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schnall R, Iribarren S.. Review and analysis of existing mobile phone applications for health care–associated infection prevention. Am J Infect Control 2015; 43 (6): 572–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sivek A, Sparnon E, Tremoulet PD.. Usability of hand hygiene observation apps. Proc Int Symp Hum Factors Ergon Health Care 2019; 8(1): 275–8. [Google Scholar]
- 34.IQVIA Institute. The growing value of digital health. 2018. https://www.iqvia.com/insights/the-iqvia-institute/reports/the-growing-value-of-digital-health. Accessed December 10, 2020.
- 35.Ali S, Lau W, McBeth J, et al. Digital manikins to self-report pain on a smartphone: a systematic review of mobile apps. Eur J Pain 2020; 25 (2): 327–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bondaronek P, Alkhaldi G, Slee A, et al. Quality of publicly available physical activity apps: review and content analysis. JMIR Mhealth Uhealth 2018; 6 (3): e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grainger R, Townsley H, White B, et al. Apps for people with rheumatoid arthritis to monitor their disease activity: a review of apps for best practice and quality. JMIR Mhealth Uhealth 2017; 5 (2): e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim B, Sharafoddini A, Tran N, et al. Consumer mobile apps for potential drug-drug interaction check: systematic review and content analysis using the Mobile App Rating Scale (MARS). JMIR Mhealth Uhealth 2018; 6 (3): e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bardus M, van Beurden S, Smith J, et al. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int J Behav Nutr Phys Act 2016; 13 (1): 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abraham C, Michie S.. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008; 27 (3): 379–87. [DOI] [PubMed] [Google Scholar]
- 42.Edwards E, Lumsden J, Rivas C, et al. Gamification for health promotion: systematic review of behaviour change techniques in smartphone apps. BMJ Open 2016; 6 (10): e012447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Michie S, Johnston M.. Behavior change techniques. In: Gellman M, Turner J, eds. Encyclopedia of Behavioural Medicine. New York: Springer; 2013. [Google Scholar]
- 44.Taj F, Klein M, van Halteren A.. Digital health behavior change technology: bibliometric and scoping review of two decades of research. JMIR Mhealth Uhealth 2019; 7 (12): e13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dugas M, Gao G, Agarwal R.. Unpacking mHealth interventions: a systematic review of behavior change techniques used in randomized controlled trials assessing mHealth effectiveness. Digit Health 2020; 6: 2055207620905411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. When and how to wash your hands. 2020. https://www.cdc.gov/handwashing/when-how-handwashing.html. Accessed February 3, 2021.
- 47.Ministry of Health NZ. Hand washing. 2020. https://www.health.govt.nz/your-health/healthy-living/good-hygiene/hand-washing. Accessed December 10, 2020.
- 48.Lalloo C, Shah U, Birnie K, et al. Commercially available smartphone apps to support postoperative pain self-management: scoping review. JMIR Mhealth Uhealth 2017; 5 (10): e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choi Y, Demiris G, Lin S, et al. Smartphone applications to support sleep self-management: review and evaluation. J Clin Sleep Med 2018; 14 (10): 1783–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Masterson Creber R, Maurer M, Reading M, et al. Review and analysis of existing mobile phone apps to support heart failure symptom monitoring and self-care management using the Mobile Application Rating Scale (MARS). JMIR Mhealth Uhealth 2016; 4 (2): e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parsippany N. IMS Institute for Healthcare Informatics: patient apps for improved healthcare: from novelty to mainstream. 2013. http://www.imshealth.com/en/thought-leadership/ims-institute/reports/patient-apps-for-improved-healthcare. Accessed October 30, 2020.
- 52.Stoyanov S, Hides L, Kavanagh D, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth 2015; 3 (1): e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stoyanov S. MARS training video. 2016. https://www.youtube.com/watch?v=25vBwJQIOcE. Accessed October 30, 2020.
- 54.Shrout P, Fleiss J.. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86 (2): 420–8. [DOI] [PubMed] [Google Scholar]
- 55.Price L, Gozdzielewska L, McAloney K.. Investigating the effect of short daily hand hygiene practice on achieving proficiency: a prospective cohort study. Antimicrob Resist Infect Control 2019; 8 (1): 156.31636899 [Google Scholar]
- 56.Baggio É, Valim M, Barbosa S, et al. Localization of the SureWash Pocket® mobile health app to Brazilian Portuguese. Rev Gaúcha Enferm 2020; 41: e20190462. [DOI] [PubMed] [Google Scholar]
- 57.GLANTA. SureWash Hand Hygiene App. 2020. https://surewash.com/surewash-app-practice-hand-hygiene/. Accessed November 19, 2020.
- 58.Essity Hygiene and Health. Hand hygiene training: VR training. 2018. https://www.tork.co.uk/hygiene/good-hygiene/tork-clean-care/healthcare/vr-training. Accessed November 19, 2020.
- 59.Javinator9889. Remember washing your hands — Handwashing reminder. 2020. https://play.google.com/store/apps/details?id=com.javinator9889.handwashingreminder&hl=en&gl=US. Accessed November 19, 2020.
- 60.Huis A, van Achterberg T, de Bruin M, et al. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implement Sci 2012; 7: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liang S, Theodoro D, Schuur J, et al. Infection prevention in the emergency department. Ann Emerg Med 2014; 64 (3): 299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Samyoun S, Shubha S, Mondol M, et al. iWash: a smartwatch handwashing quality assessment and reminder system with real-time feedback in the context of infectious disease. Smart Health (Amst) 2021; 19: 100171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nahum-Shani I, Smith S, Spring B, et al. Just-in-Time Adaptive Interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med 2018; 52 (6): 446–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were generated or analyzed in support of this research.