Highlights
-
•
Chain of pathogen transmission between individual donor and recipient is modeled.
-
•
Related pairs of efficient and inefficient ‘airborne’ pathogens are contrasted.
-
•
Drivers operate on tissue, individual, community, country, and global levels.
-
•
Pandemic risk is heightened by pathogen evolution and changes in host interaction.
-
•
Ultimate drivers include socio-economic developments and climate changes.
Abstract
Airborne pathogens — either transmitted via aerosol or droplets — include a wide variety of highly infectious and dangerous microbes such as variola virus, measles virus, influenza A viruses, Mycobacterium tuberculosis, Streptococcus pneumoniae, and Bordetella pertussis. Emerging zoonotic pathogens, for example, MERS coronavirus, avian influenza viruses, Coxiella, and Francisella, would have pandemic potential were they to acquire efficient human-to-human transmissibility. Here, we synthesize insights from microbiological, medical, social, and economic sciences to provide known mechanisms of aerosolized transmissibility and identify knowledge gaps that limit emergency preparedness plans. In particular, we propose a framework of drivers facilitating human-to-human transmission with the airspace between individuals as an intermediate stage. The model is expected to enhance identification and risk assessment of novel pathogens.
Current Opinion in Virology 2017, 22:22–29
This review comes from a themed issue on Emerging viruses: intraspecies transmission
Edited by Ron A.M Fouchier and Lin-Fa Wang
For a complete overview see the Issue and the Editorial
Available online 2nd December 2016
http://dx.doi.org/10.1016/j.coviro.2016.11.006
1879-6257/© 2016 The Author(s). Published by Elsevier B.V. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/).
Introduction
The horror of airborne infectious diseases subsided substantially in the 20th century in developed nations, largely due to implementation of hygiene practices and the development of countermeasures such as vaccination and antimicrobials. The recent emergence of zoonotic pathogens such as avian influenza A viruses (e.g. H5N1 and H7N9) and coronaviruses (CoV) (i.e. SARS CoV (severe acute respiratory syndrome) and MERS CoV (Middle East respiratory syndrome)) raises the specter of future pandemics with unprecedented health and economic impacts if these pathogens gain the ability to spread efficiently between humans via the airborne route. While cross-species barriers have helped avoid a human pandemic with highly pathogenic avian influenza A (HPAI) viruses, a limited number of mutations in circulating avian H5N1 viruses would be needed for the acquisition of airborne transmissibility in mammals [1•]. A global pandemic by SARS CoV was averted largely by fast identification, rapid surveillance and effective quarantine practices. However, not all emerging pathogens can be contained due to a delay in initial detection, an inability to properly assess pandemic risk, or an inability to contain an outbreak at the point of origin. Before 2009, widely circulating H1N1 swine viruses were largely thought to pose little pandemic risk but, despite early attempts to limit spread, pH1N1 caused the first influenza virus pandemic of the 21st century. Implementation of suitable countermeasures is hampered by our limited capability to anticipate the sequence of events following the initial detection of a novel microorganism in an animal or human host. In the immediate future, the occurrence of (i.e. frequency of spill-over events from an animal to the human population), the detection of (i.e. diagnostic capabilities), and the awareness for (i.e. likelihood of public health services to recognize) novel epidemic agents will likely increase qualitatively and quantitatively. Updating of emergency preparedness plans in an evidence-guided process requires an interdisciplinary concept of research and public health efforts taking into account the multifactorial nature of the problem to aid policy formulation [2]. Here we build on a conceptual framework for the classification of drivers of human exposure to animal pathogens [3••] and suggest a framework of drivers determining the efficiency of human-to-human transmission involving the airspace.
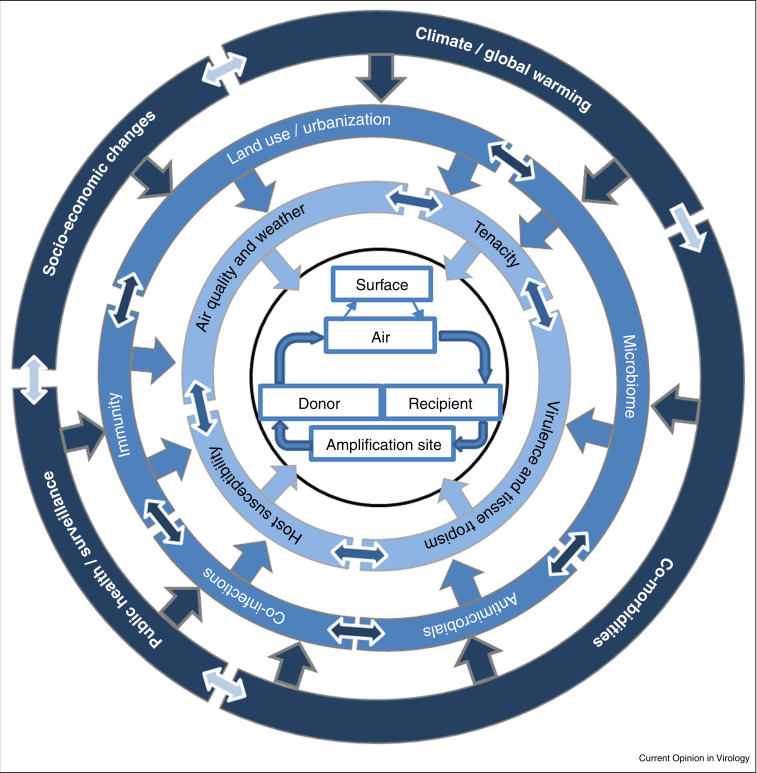
Circle of transmission events
The airborne transmission of pathogens occurs through ‘aerosol’ and ‘droplet’ means [4, 5••]. In a strict sense, airborne transmission refers to aerosols (≤5 μm) that can spread over distances greater than 1 m, while droplet transmission is defined as the transfer of large-particle droplets (>5 μm) over a shorter distance [5••]. Here, we consider airborne transmission of infectious agents in a broader sense as any transmission through the air which consists of four steps (Figure 1 ): Firstly, the pathogen is associated with either liquid droplets/aerosols or dust particles when traveling directly from donor to recipient, but may also be deposited on a surface and re-emerge into the air later; secondly, the pathogen is deposited in the recipient, usually by inhalation, resulting in infection of the respiratory tract; thirdly, the pathogen is amplified, either in the respiratory tract or in peripheral tissues; and finally, the pathogen is emergent at the site of shedding (in most cases the upper respiratory tract) in sufficient loads and capable of expulsion. In the process of transmission, the recipient becomes a donor when microbial replication and subsequent pathophysiological events in the host result in release of the pathogen.
Figure 1.
Circle of events leading to human-to-human transmission of airborne pathogens. (1) The pathogen is associated with either small aerosols/large droplets or dust particles when transported through the air from donor to recipient. This may be directly, or via an intermediate stage involving settlement on a surface and re-emergence into the air later. (2) A low infectious dose is sufficient for deposition of the pathogen in the respiratory tract of the recipient. (3) After infection of susceptible cells, pathogens may amplify at the site of deposition only (localized site), or are disseminated from the primary deposition site to peripheral tissues (secondary site) where additional amplification takes place. (4) Eventually, the recipient becomes the donor and pathogens are expelled from the exit site. This is (usually) the respiratory tract, but may also be the secondary site of replication. High infectious loads of the pathogen emerge in the air, and the transmission cycle is repeated.
Drivers impacting on movement of pathogens through the air
Airborne transmission of microbes can follow different aerodynamic principles, and some microorganisms are suspected or proven to spread by more than one route [4]. Moreover, the mode of transmission and anisotropic delivery of a pathogen into the recipient contributes to disease severity [6, 7]. There are no substantive differences between droplet-size distribution for expulsive methods like sneezing, cough with mouth closed, cough with mouth open, and speaking loudly one hundred words [8, 9, 10]; however, the number of respiratory droplets that likely contain pathogens can differ [9]. After expulsion, successful transmission requires that the pathogen remains infectious throughout airborne movement, with or without an intervening deposition event (Figure 1). Drivers influencing the success of such a process are those that define the chemico-physical properties of both the air mass and the vehicle or carrier, including temperature, ultraviolet (UV) radiation, relative (RH) and absolute humidity, and air ventilation (inside) or air movement (outside) [9]. Their interplay ultimately determines pathogen movement and stability [11, 12, 13]. Pathogen survival is also influenced by pathogen structure, for example, enveloped viruses are less stable outside the host than non-enveloped viruses [14]. Among Chlamydia (Ch.) pneumoniae, Ch. trachomatis LGV2, Streptococcus (S.) pneumoniae, S. faecalis, Klebsiella pneumoniae, and cytomegalovirus, the survival of Ch. pneumoniae (and S. faecalis) in aerosols was superior [15]. Variation in RH might influence not only environmental stability of the pathogen but also the droplet size [16] which in turn defines deposition rate [16, 17]. Eighty percent of droplets emitted from a cough deposit within 10 min, and highest deposition rates for all droplet-nuclei sizes range within 1 m horizontal distance [17]. Pathogens like influenza virus can persist in the environment for hours to days and have been found on surfaces in healthcare settings [18, 19, 20, 21]. UV radiation is the major inactivating factor for influenza viruses in the outdoor environment (reviewed in [22]).
Drivers impacting on the infection of the recipient
Pathogen-containing large particles (>6 μm) deposit predominantly in the upper airway, medium-sized particles (2–6 μm) mainly in central and small airways, and small particles (<2 μm) predominantly in the alveolar region of the lungs [23]. In general, airborne pathogens tend to have a relatively low infectious dose 50% (ID50) value. At any specific site of deposition within a host, ID50 of a pathogen is determined by factors such as local immune responses and the cellular and tissue tropism defined by distribution of receptors and/or adherence factors, tissue temperature, pH, polymerase activity of the pathogen, and activating proteases. Co-infections may alter immune responses and factors that govern tropism.
Drivers impacting on pathogen amplification in the host
Pathogens amplify either at the site of initial deposition in the respiratory tract or in peripheral tissues. For influenza virus or human respiratory syncytial virus, this is the site of initial entry whilst other pathogens have either distinct secondary amplification sites or replicate both locally and systemically, for example, Measles virus (MeV), Nipah virus and Mycobacterium (M.) tuberculosis (Figure 1).
Microorganisms often damage host tissue through the release of toxins and toxic metabolites, as a direct result of replication, or as a consequence of activation and infiltration of immune cells [24••]. This may allow the pathogen to spread in the body and replicate to sufficient numbers to favor onward transmission. Self-assembly in highly organized, surface-attached, and matrix encapsulated structures called biofilms enhances microbial survival in stressful environments [25•] and may even harbor drug-tolerant populations. Biofilms of M. tuberculosis can contain resistant populations that persist despite exposure to high levels of antibiotics [26]. A third strategy is followed by many human pathogens that have at some stage evolved or acquired a range of mechanisms allowing host immune antagonism [27, 28•] to successfully replicate to high loads in the presence of innate and/or adaptive immunity [29]. However, several rounds of stuttering chains of transmission may be required before a pathogen can successfully emerge into a new host population. Multiple forays of the pathogen into the population may serve to create a level of immunity, thus establishing conditions favoring more prolonged outbreaks following a reintroduction of the infectious agent [30, 31] which then enables sustained pathogen/human host co-evolution.
Evolution to allow host adaptation and/or airborne transmissibility can be driven by changes in pathogen population genetics at the consensus level but also by genetic variability of the entire population. RNA viruses exist as a population of closely related genetic variants within the host. The ability of a pathogen to generate a genetically diverse population is considered critical to allow adaption when faced with a range of selective pressures [32, 33]. High-fidelity poliovirus mutants that produce viral populations with little genetic diversity are attenuated despite apparent overall identical consensus sequences to wildtype strains [34, 35, 36]. Factors enabling acquisition of novel traits through high mutation rate, and/or a propensity to acquire novel genetic material through re-assortment or recombination are important drivers at the level of pathogen replication, amplification and adaptation within the host. Bacteria additionally deploy transfer of mobile genetic elements (plasmids, transposons and bacteriophages) to acquire novel virulence factors, toxins and/or antimicrobial resistance. Microbial adaptation by drug resistance is often attained at the cost of decreased fitness, as illustrated by a reduced growth rate of M. tuberculosis strains resistant to isoniazid [37], but multi-drug resistant (MDR) strains can be up to 10 times more or 10 times less transmissible than pan-susceptible strains [38]. Heredity of susceptibility on the host side enhances the risk of disease and transmission, as seen historically with the selection of populations with innate tuberculosis resistance by the evolutionary pressure of several, hundred-year-old epidemics in Europe and North America [39, 40, 41].
Drivers impacting on pathogen expulsion by the donor
The high viral load in the upper respiratory tract combined with a strong cough reflex drives efficient host-to-host human transmission of MeV [42]. At the level of virus amplification in host epithelia, lesions are observed in the later stages of disease as well as extensive infiltration of infected tissue by immune cells. It is currently unclear to what extent the host immune response contributes to formation of pathological lesions and to the transmissibility of the virus. Levels of exhalation of infected particles significantly vary interpersonally [43••], for example, for M. tuberculosis [44] and for influenza A virus [45], both in healthy and in virus-infected persons [10, 46], as well as intra-individually over time [47]. Drivers of airborne transmissibility appear to be closely linked to disease progression and severity, to the incubation period and onset of symptoms in M. tuberculosis [48].
Framework for the classification of drivers
Determinants that confer efficient airborne transmissibility for zoonotic pathogens among humans, thus permitting pandemic emergence, can be defined as qualitative or quantitative changes in key factors that govern one or more of the four stages of the transmission circle. The sum of changes in spatial and temporal terms that facilitate or limit the progression to successive stages of the circle corresponds to the evolution of emerging pathogens. To predict the likelihood that a certain pathogen identified in, or next to, a human being (index patient) will become a pandemic threat, a multilevel framework of drivers has to be considered. Categorized in a descriptive manner, drivers may act at the level of cells and tissues, of individuals, communities and countries, or even on a global scale. However, drivers are highly interactive and may be effective at different scales or levels. As an example, host susceptibility might be directly encoded for in the host genome (e.g. by the presence or absence, by the expression or silencing of genes encoding for pathogen receptors). Once the transmitted pathogen finds an entry into such a susceptible human host, its interaction with the host immune system ultimately determines whether infection is established and whether it progresses to a point where onward transmission to a new host is facilitated. These interactions are influenced at the individual or host level by other drivers governing an immune response. These drivers in turn may include the host genetic background as genetic entities impact on the kind of immune response (e.g. Th1 versus Th2 bias) developed by an individual or a group of individuals within a population. Pre-existing immunity or the presence of concurrent infections or disruption to the normal functioning of the immune system including co-morbidities which may represent more distal drivers or in turn modulate more distal drivers, play important roles. With effective treatment, the contagiousness of a particular disease may be reduced not only by decreasing the number of the pathogens in the infected site and those that will be expectorated but also by introducing, for example, antibiotic into the infectious droplet nuclei [49]. Many drivers are acting at the tissue or individual level but are themselves subject to modification at the community level by, for example, the frequency and intensity of social contact and the composition of the group a person is interacting with, for example, in terms of health and hygiene standard and age distribution. Examples are tuberculosis in the working class in the age of industrialization and the Spanish flu during World War I. More distal factors are relevant at the country level including (the variability of) host population genetics (susceptibility of the population as a whole), demography, public health strategies for treatment or vaccination or access to medical care, which are likewise, to some extent, governed by socio-economic drivers. Air pollution, land use, urbanization and socio-economic changes are important drivers of emergence of airborne infections at the supranational level. Although human population densities have continued to rise and reach unprecedented levels, airborne diseases of public concern in developed countries in the second half of the 20th century have typically comprised relatively self-limiting or preventable diseases like the common cold, seasonal flu and MeV. Continuous developments like agglomeration of settlement areas in developing countries, along with urbanization and rural depopulation, and exponentially increasing human movement in numbers and distances on a global scale, however, may outpace contemporary achievements in disease prevention. Climatic changes also occur at a global level, which could have serious impact on infectious diseases in humans and animals [50]. Extreme weather conditions alter seasonal patterns of emergence and expansion of diseases even though direct proof for the influence of climate change on regional, national, supranational or global level on the emergence of new or frequency of established infections is difficult to obtain. To mirror the complexity of the problem we suggest a concise and weighted framework of drivers (Figure 2 ) taking into consideration different levels, from cell and tissue through to global scale but also the multitude of influences between these levels. While some drivers at an outer level may only imprint on one driver in the level below, other drivers can impact several lower level drivers and in sum may be equally important to drivers considered to act from an outer level. Classification of drivers as acting at a more proximal or more distal level also is not exclusive and inverted imprinting may occur under several circumstances as outlined above.
Figure 2.
Framework for the classification of drivers of human-to-human transmission of zoonotic pathogens by the airborne route (interhuman barrier). These drivers operate on tissue, individual, community, country, and global levels. The presented framework also makes provisions for the multitude of influences between levels highlighting that some drivers have implications for several lower level drivers and in sum may be equally important to drivers considered to act from an outer level.
Knowledge gaps and future prospect
Despite decades of research on ‘airborne transmission factors’, surprisingly few quantitative data is available for factors impacting the majority of infectious diseases that transmit via this route. Furthermore, for some microorganisms, for example, for coronaviruses, epidemiological or experimental evidence that transmission of the pathogens via the airborne route is successful or even contributes importantly to epidemic or pandemic spread of the agent remains weak. A large body of work is focused on influenza viruses and the indoor environment, likely because perturbations of the indoor pathogen transmission ecosystem are easier to generate and quantify. Published studies assessing viable pathogen counts directly from subject's respiratory maneuvers are restricted to a few respiratory pathogens (influenza A virus, M. tuberculosis, P. aeruginosa, S. pyogenes). Evaluation of factors underlying the highly variable levels of pathogen shedding, for example, by long-term examination of individuals to determine how pathogen load changes during infection of the respiratory tract with different viruses and bacterial species are urgently needed. Current technical developments may open novel experimental opportunities [51•]. When designing such studies, consideration of zoonotic and human-specific pathogens as well as delineating strategies employed by both viruses and bacterial pathogens will help to identify commonalities in the strategies followed by successful airborne pathogens. Especially investigation of organisms assumed to have no capacity of human-to-human transmission via the airborne route in suitable animal models will help explain why some pathogens, despite having a very low infectious dose, are likely not directly transmitted from infected persons. Examples would be the human-to-human transmission of Yersinia pestis versus Francisella tularensis, or the assessment why Legionella pneumophila transmission can occur over long distances from artificial sources [52], but usually not inter-personally (with the exception of a first described case [53]).
Beyond representing an ever-increasing ethical and economic burden, the recent more frequent occurrence of zoonotic pathogens in the human population also inheres in the unique opportunity to further our knowledge of the prerequisites for airborne pandemic spread. Genomics-based methods have already allowed a significant advance in our understanding of the evolution and spread of bacterial pathogens. In the developed world, whole genome sequencing is being established for routine use in clinical microbiology, both for tracking transmission and spread of pathogens, as well as prediction of drug-resistance profiles, allowing rapid outbreak detection and analysis in almost real-time, as evolution occurs in the wild [54••]. Except for influenza A viruses, genetic correlates (surrogates) of the ability of a zoonotic pathogen to efficiently overcome the interspecies barrier and allow rapid spread within the human population are poorly defined. Any emergence of novel molecular patterns in microorganisms results from an evolutionary process driven by factors not encoded for in genomes and determined by the frequencies of genome alterations occurring under natural conditions. The broad introduction of ‘omic's’ technologies, advances in global data exchange capabilities and the advent of (bio)informatic tools allowing processing of large data collections (‘big data’) have put the technical capacity to integrate phenotypic data from clinical, from epidemiological and from experimental studies in vitro and in vivo at our disposal, with relevant target species like livestock in particular, and allow genome-wide association studies. Deploying the categorization of drivers and the relative level of their impact as suggested herein will allow for a weighting of the different drivers in the specific framework for any particular pathogen, and help to predict the pandemic potential of airborne pathogens.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Acknowledgements
The expert workshop was financially supported by the European Commission (FP7 programme in the framework of the project ‘Antigone — ANTIcipating the Global Onset of Novel Epidemics’, project number 278976). The research of SH is funded by an NWO VIDI grant (contract number 91715372). The sponsors had no role in the collection, analysis and interpretation of data, in the writing of the report; and in the decision to submit the article for publication.
References
- 1•.Linster M., van Boheemen S., de Graaf M., Schrauwen E.J.A., Lexmond P., Mänz B., Bestebroer T.M., Baumann J., van Riel D., Rimmelzwaan G.F. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell. 2014;157:329–339. doi: 10.1016/j.cell.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors show the phenotypic properties required for a fully avian highly pathogenic A/H5N1 influenza virus to become airborne-transmissible in the ferret transmission model.
- 2.Coker R., Rushton J., Mounier-Jack S., Karimuribo E., Lutumba P., Kambarage D., Pfeiffer D.U., Stärk K., Rweyemamu M. Towards a conceptual framework to support one-health research for policy on emerging zoonoses. Lancet Infect Dis. 2011;11:326–331. doi: 10.1016/S1473-3099(10)70312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3••.Gortazar C., Reperant L.A., Kuiken T., de la Fuente J., Boadella M., Martínez-Lopez B., Ruiz-Fons F., Estrada-Peña A., Drosten C., Medley G. Crossing the interspecies barrier: opening the door to zoonotic pathogens. PLoS Pathog. 2014;10:e1004129. doi: 10.1371/journal.ppat.1004129. [DOI] [PMC free article] [PubMed] [Google Scholar]; Article provides the conceptual framework of drivers this review is built upon.
- 4.Bunyan D., Ritchie L., Jenkins D., Coia J.E. Respiratory and facial protection: a critical review of recent literature. J Hosp Infect. 2013;85:165–169. doi: 10.1016/j.jhin.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5••.Fernstrom A., Goldblatt M. Aerobiology and its role in the transmission of infectious diseases. J Pathog. 2013;2013:493960. doi: 10.1155/2013/493960. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review of aerobiological variables affecting airborne transmission and common origin of infectious particles.
- 6.Milton D.K. What was the primary mode of smallpox transmission? Implications for biodefense. Front Cell Infect Microbiol. 2012;2:150. doi: 10.3389/fcimb.2012.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burke C.W., Bridges O., Brown S., Rahija R., Russell C.J. Mode of parainfluenza virus transmission determines the dynamics of primary infection and protection from reinfection. PLoS Pathog. 2013;9:e1003786. doi: 10.1371/journal.ppat.1003786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loudon R.G., Roberts R.M. Droplet expulsion from the respiratory tract. Am Rev Respir Dis. 1967;95:435–442. doi: 10.1164/arrd.1967.95.3.435. [DOI] [PubMed] [Google Scholar]
- 9.Duguid J.P. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. J Hyg. 1946;44:471–479. doi: 10.1017/s0022172400019288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papineni R.S., Rosenthal F.S. The size distribution of droplets in the exhaled breath of healthy human subjects. J Aerosol Med. 1997;10:105–116. doi: 10.1089/jam.1997.10.105. [DOI] [PubMed] [Google Scholar]
- 11.Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowen A.C., Mubareka S., Steel J., Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steel J., Palese P., Lowen A.C. Transmission of a 2009 pandemic influenza virus shows a sensitivity to temperature and humidity similar to that of an H3N2 seasonal strain. J Virol. 2010;85:1400–1402. doi: 10.1128/JVI.02186-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polozov I.V., Bezrukov L., Gawrisch K., Zimmerberg J. Progressive ordering with decreasing temperature of the phospholipids of influenza virus. Nat Chem Biol. 2008;4:248–255. doi: 10.1038/nchembio.77. [DOI] [PubMed] [Google Scholar]
- 15.Theunissen H.J., Lemmens-den Toom N.A., Burggraaf A., Stolz E., Michel M.F. Influence of temperature and relative humidity on the survival of Chlamydia pneumoniae in aerosols. Appl Environ Microbiol. 1993;59:2589–2593. doi: 10.1128/aem.59.8.2589-2593.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang W., Marr L.C. Dynamics of airborne influenza A viruses indoors and dependence on humidity. PLoS ONE. 2011;6:e21481. doi: 10.1371/journal.pone.0021481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng Y.H., Wang C.H., You S.H., Hsieh N.H., Chen W.Y., Chio C.P., Liao C.M. Assessing coughing-induced influenza droplet transmission and implications for infection risk control. Epidemiol Infect. 2016;144:333–345. doi: 10.1017/S0950268815001739. [DOI] [PubMed] [Google Scholar]
- 18.Bean B., Moore B.M., Sterner B., Peterson L.R., Gerding D.N., Balfour H.H., Jr. Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146:47–51. doi: 10.1093/infdis/146.1.47. [DOI] [PubMed] [Google Scholar]
- 19.Boone S.A., Gerba C.P. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol. 2007;73:1687–1696. doi: 10.1128/AEM.02051-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edward D.F.F. Resistance of influenza virus to drying and its demonstration on dust. Lancet. 1941;238:664–666. [Google Scholar]
- 21.Tiwari A., Patnayak D.P., Chander Y., Parsad M., Goyal S.M. Survival of two avian respiratory viruses on porous and nonporous surfaces. Avian Dis. 2006;50:284–287. doi: 10.1637/7453-101205R.1. [DOI] [PubMed] [Google Scholar]
- 22.Weber T.P., Stilianakis N.I. Inactivation of influenza A viruses in the environment and modes of transmission: a critical review. J Infect. 2008;57:361–373. doi: 10.1016/j.jinf.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darquenne C. Aerosol deposition in health and disease. J Aerosol Med Pulm Drug Deliv. 2012;25:140–147. doi: 10.1089/jamp.2011.0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24••.Méthot P.O., Alizon S. What is a pathogen? Toward a process view of host–parasite interactions. Virulence. 2014;5:775–785. doi: 10.4161/21505594.2014.960726. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review of pathogenicity/virulence as a dynamical feature of an interaction between a host and microbes.
- 25•.Gupta P., Sarkar S., Das B., Bhattacharjee S., Tribedi P. Biofilm, pathogenesis and prevention — a journey to break the wall: a review. Arch Microbiol. 2016;198:1–15. doi: 10.1007/s00203-015-1148-6. [DOI] [PubMed] [Google Scholar]; Review of biofilm formation, possible mechanisms of drug resistance in biofilms and recent therapeutic approaches involved in successful eradication of biofilms.
- 26.Ojha A.K., Baughn A.D., Sambandan D., Hsu T., Trivelli X., Guerardel Y., Alahari A., Kremer L., Jacobs W.R., Jr., Hatfull G.F. Growth of Mycobacterium tuberculosis biofilms containing free mycolic acids and harbouring drug-tolerant bacteria. Mol Microbiol. 2008;69:164–174. doi: 10.1111/j.1365-2958.2008.06274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pieters J. Mycobacterium tuberculosis and the macrophage: maintaining a balance. Cell Host Microbe. 2008;3:399–407. doi: 10.1016/j.chom.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 28•.Chiang J.J., Davis M.E., Gack M.U. Regulation of RIG-I-like receptor signaling by host and viral proteins. Cytokine Growth Factor Rev. 2014;25:491–505. doi: 10.1016/j.cytogfr.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review covering recent progress in our knowledge of the regulation of cellular antiviral signaling pathways by host factors and viral antagonistic proteins.
- 29.Nuermberger E., Bishai W.R., Grosset J.H. Latent tuberculosis infection. Semin Respir Crit Care Med. 2004;25:317–336. doi: 10.1055/s-2004-829504. [DOI] [PubMed] [Google Scholar]
- 30.Pulliam J.R.C., Epstein J.H., Dushoff J., Rahman S.A., Bunning M., Jamaluddin A.A., Hyatt A.D., Field H.E., Dobson A.P., Daszak P. Agricultural intensification, priming for persistence and the emergence of Nipah virus: a lethal bat-borne zoonosis. J R Soc Interface. 2011;9:89–101. doi: 10.1098/rsif.2011.0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pulliam J.R.C., Dushoff J.G., Levin S.A., Dobson A.P. Epidemic enhancement in partially immune populations. PLoS ONE. 2007;2:e165. doi: 10.1371/journal.pone.0000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bordería A.V., Stapleford K.A., Vignuzzi M. RNA virus population diversity: implications for inter-species transmission. Curr Opin Virol. 2011;1:643–648. doi: 10.1016/j.coviro.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 33.Lancaster K.Z., Pfeiffer J.K. Viral population dynamics and virulence thresholds. Curr Opin Microbiol. 2012;15:525–530. doi: 10.1016/j.mib.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pfeiffer J.K., Kirkegaard K. Increased fidelity reduces poliovirus fitness and virulence under selective pressure in mice. PLoS Pathog. 2005;1:e11. doi: 10.1371/journal.ppat.0010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vignuzzi M., Stone J.K., Arnold J.J., Cameron C.E., Andino R. Quasispecies diversity determines pathogenesis through cooperative interactions in a viral population. Nature. 2005;439:344–348. doi: 10.1038/nature04388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meng T., Kwang J. Attenuation of human enterovirus 71 high-replication-fidelity variants in AG129 mice. J Virol. 2014;88:5803–5815. doi: 10.1128/JVI.00289-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gagneux S. Fitness cost of drug resistance in Mycobacterium tuberculosis. Clin Microbiol Infect. 2009;15:66–68. doi: 10.1111/j.1469-0691.2008.02685.x. [DOI] [PubMed] [Google Scholar]
- 38.Borrell S., Gagneux S. Infectiousness, reproductive fitness and evolution of drug-resistant Mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2009;13:1456–1466. [PubMed] [Google Scholar]
- 39.Stead W.W., Senner J.W., Reddick W.T., Lofgren J.P. Racial differences in susceptibility to infection by Mycobacterium tuberculosis. N Engl J Med. 1990;322:422–427. doi: 10.1056/NEJM199002153220702. [DOI] [PubMed] [Google Scholar]
- 40.Crowle A.J., Elkins N. Relative permissiveness of macrophages from black and white people for virulent tubercle bacilli. Infect Immun. 1990;58:632–638. doi: 10.1128/iai.58.3.632-638.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stead W.W. Genetics and resistance to tuberculosis. Could resistance be enhanced by genetic engineering? Ann Intern Med. 1992;116:937–941. doi: 10.7326/0003-4819-116-11-937. [DOI] [PubMed] [Google Scholar]
- 42.Ludlow M., McQuaid S., Milner D., de Swart R.L., Duprex W.P. Pathological consequences of systemic measles virus infection. J Pathol. 2015;235:253–265. doi: 10.1002/path.4457. [DOI] [PubMed] [Google Scholar]
- 43••.Lloyd-Smith J.O., Schreiber S.J., Kopp P.E., Getz W.M. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]; An integrated theoretical and statistical analysis of the influence of individual variation in infectiousness on disease emergence. The authors conclude that superspreading is a normal feature of infectious diseases.
- 44.Jones-López E.C., Namugga O., Mumbowa F., Ssebidandi M., Mbabazi O., Moine S., Mboowa G., Fox M.P., Reilly N., Ayakaka I. Cough aerosols of Mycobacterium tuberculosis predict new infection: a household contact study. Am J Respir Crit Care Med. 2013;187:1007–1015. doi: 10.1164/rccm.201208-1422OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9:e1003205. doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fabian P., Brain J., Houseman E.A., Gern J., Milton D.K. Origin of exhaled breath particles from healthy and human rhinovirus-infected subjects. J Aerosol Med Pulm Drug Deliv. 2011;24:137–147. doi: 10.1089/jamp.2010.0815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wurie F., Le Polain de Waroux O., Brande M., Dehaan W., Holdgate K., Mannan R., Milton D., Swerdlow D., Hayward A. Characteristics of exhaled particle production in healthy volunteers: possible implications for infectious disease transmission. F1000Res. 2013;2:14. doi: 10.12688/f1000research.2-14.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wurie F.B., Lawn S.D., Booth H., Sonnenberg P., Hayward A.C. Bioaerosol production by patients with tuberculosis during normal tidal breathing: implications for transmission risk. Thorax. 2016;71:549–554. doi: 10.1136/thoraxjnl-2015-207295. [DOI] [PubMed] [Google Scholar]
- 49.Sepkowitz K.A. How contagious is tuberculosis? Clin Infect Dis. 1996;23:954–962. doi: 10.1093/clinids/23.5.954. [DOI] [PubMed] [Google Scholar]
- 50.Friedrich B., Hacker J., Hasnain S.E., Mettenleiter T.C., Schell J., editors. Climate Change and Infections Diseases. Nova Acta Leopoldina; 2010. [Google Scholar]
- 51•.Fronczek C.F., Yoon J.-Y. Biosensors for monitoring airborne pathogens. J Lab Autom. 2015;20:390–410. doi: 10.1177/2211068215580935. [DOI] [PubMed] [Google Scholar]; Review of current laboratory-based methods to monitor airborne pathogens.
- 52.Nguyen T.M., Ilef D., Jarraud S., Rouil L., Campese C., Che D., Haeghebaert S., Ganiayre F., Marcel F., Etienne J. A community-wide outbreak of legionnaires disease linked to industrial cooling towers — how far can contaminated aerosols spread? J Infect Dis. 2006;193:102–111. doi: 10.1086/498575. [DOI] [PubMed] [Google Scholar]
- 53.Correia A.M., Ferreira J.S., Borges V., Nunes A., Gomes B., Capucho R., Gonçalves J., Antunes D.M., Almeida S., Mendes A. Probable person-to-person transmission of Legionnaires’ disease. N Engl J Med. 2016;374:497–498. doi: 10.1056/NEJMc1505356. [DOI] [PubMed] [Google Scholar]
- 54••.Bentley S.D., Parkhill J. Genomic perspectives on the evolution and spread of bacterial pathogens. Proc Biol Sci. 2015;282:20150488. doi: 10.1098/rspb.2015.0488. [DOI] [PMC free article] [PubMed] [Google Scholar]; Summarizing impact and options of whole genome sequencing implemented in clinical microbiology for our understanding of pathogen evolution and epidemiology.